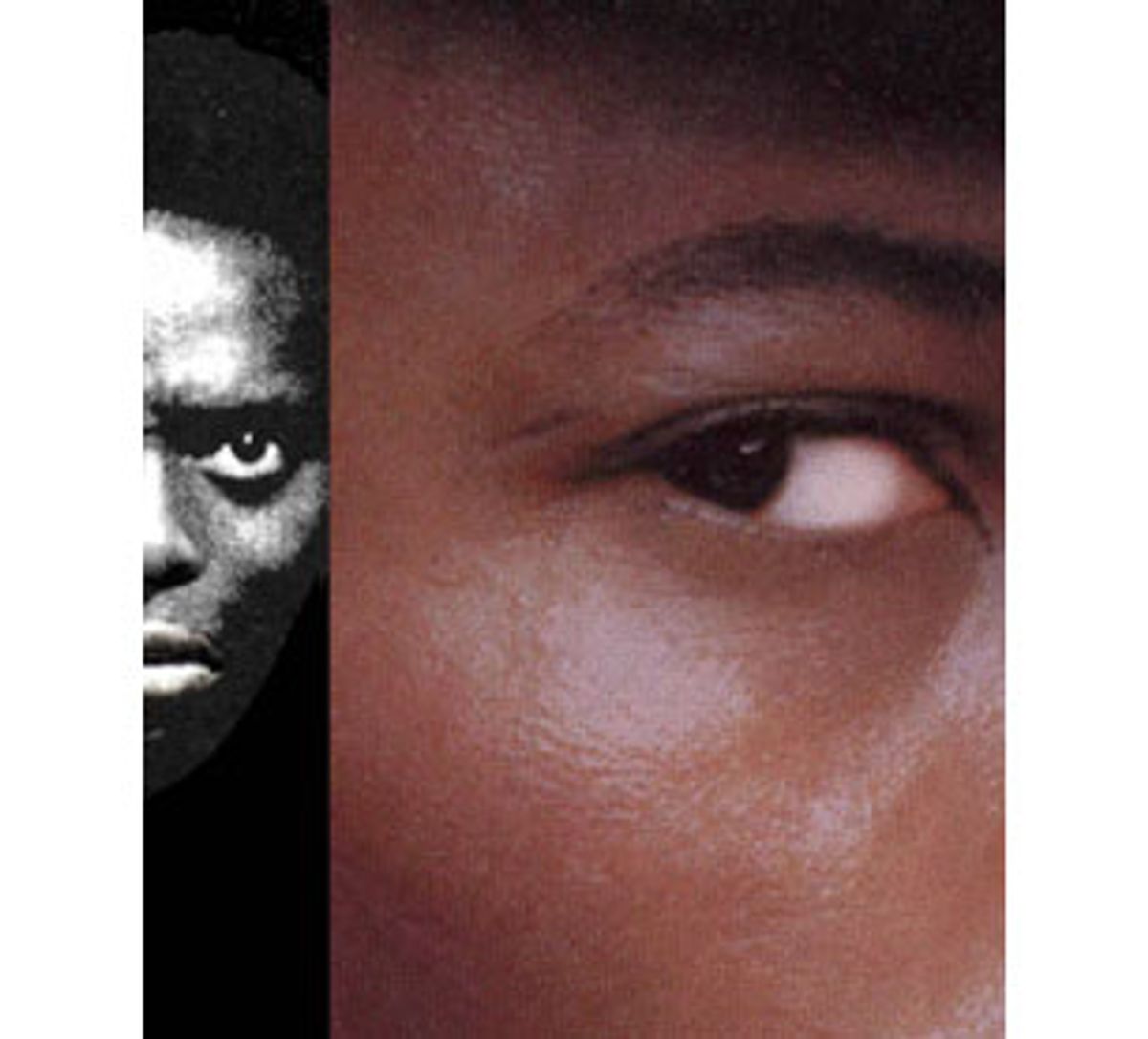
It took only a few weeks on the job for William Lawson to notice that there was something very strange going on. The psychiatrist had just joined the staff of the John L. McClellan Veterans Hospital in North Little Rock, Ark., and already he had seen patient after patient -- dozens of them, as it turned out -- with the same ill-fitting diagnosis. All African-American men, all veterans of combat in the Vietnam War, they suffered from terrifying nightmares, gut-twisting anxiety, flashbacks of fighting -- classic symptoms of post-traumatic stress disorder (PTSD). Yet they'd been assigned a very different condition: schizophrenia.
Lawson immediately took the men off the anti-psychotic medication they'd been prescribed, replacing it with the psychotherapy and antidepressants that have proven effective in relieving PTSD. Under the new treatment regime, most of the patients made a quick recovery.
Mistakes like the ones he discovered may be odd, but they're far from uncommon, says Lawson, now a professor at Indiana University and the co-editor of "Cross-Cultural Psychiatry" (Wiley, 1999). Studies going back to the 1960s show that African-Americans are significantly more likely to be diagnosed with schizophrenia than whites, a discrepancy due at least in part to clinician error. The rates of such mislabeling vary with the type of facility -- they're much lower, for example, in hospitals affiliated with universities -- but Lawson estimates that in overburdened community mental-health centers, as many as 30 percent of black patients diagnosed with schizophrenia actually have some other illness.
Of course, whites are also misdiagnosed at times, but far less frequently. According to Stephen Strakowski, M.D., a psychiatrist at the University of Cincinnati who has studied the issue, blacks are two to five times more likely than whites to be misidentified as schizophrenic. Ethnicity affects the diagnosis of other mental illnesses as well; clinicians sometimes miss the signs of major depression and bipolar disorder in blacks, for example, thereby leading to underdiagnosis. But schizophrenia presents special problems.
For one thing, it's precisely these bipolar and depressive patients who are likely to be misdiagnosed with schizophrenia. Each disease is treated with a different type of medication and the drugs used to manage schizophrenia have unfortunate side effects, including the involuntary (and sometimes permanent) twitching of facial muscles known as tardive dyskinesia. "The worst side effects accrue as you get more medicine over time," Strakowski observes. "We really want to minimize that, and only expose people who really have to have it."
While they wait for their misdiagnoses to be corrected, patients who actually have a different illness may be getting sicker, increasing the risk that they will attempt suicide and decreasing the odds that they'll eventually get better. (The more untreated episodes of mania and depression experienced by bipolar patients, for example, the tougher they are to treat when they do get appropriate care.) No less of a concern is the stigma attached to schizophrenia, a severe and probably partly inherited disorder of the brain that bears heavy social baggage. People diagnosed with schizophrenia are frequently feared or shunned by others, and have difficulty finding employment and housing. Studies suggest that schizophrenics often receive substandard medical care for illnesses like diabetes or high blood pressure because their physical complaints are dismissed as a product of their craziness.
But why would black people be more likely to be tagged as schizophrenics? Experts have some ideas; the first is simple racism. While clinicians are hesitant to burden middle- or upper-class whites with a devastating diagnosis like schizophrenia, Rosemary Farmer, Ph.D., assistant professor of social work at Virginia Commonwealth University, observes, such considerations don't always apply to minorities. "With an African-American, especially a lower socioeconomic-status African-American, people don't care as much, somehow," she says. "It's like, 'Oh well, what difference does it make, we'll label them anything.'"
Such careless -- or deliberate -- labeling has a long and ugly history. In the years before the Civil War, inflated estimates of mental illness among free blacks were used by anti-abolitionists to "prove" that blacks were better off as slaves. Even into the 1950s, American psychiatry maintained that blacks were too psychologically simple or too "jovial" to be depressed -- and so diagnosed the bulk of their mental illness as schizophrenia.
A second explanation is somewhat more benign. Clinicians unfamiliar with African-American culture and history may misread a black patient's signals, interpreting discomfort with an overwhelmingly white mental-health institution, for example, as paranoia. The psychiatrists who had diagnosed the Arkansas veterans' PTSD as schizophrenia "were unaware of the substantial role that African-Americans played in combat in Vietnam and the frequency of the disorder among African-Americans," Lawson reports. "They weren't even getting the patients' combat histories."
The ostensibly objective diagnostic tools on which doctors rely may themselves be biased against blacks. Strakowski notes that the entry on schizophrenia in the clinician's bible, the DSM-IV, instructs the diagnostician to look first for the presence of hallucinations and delusions. Mentally ill African-Americans "tend to have more severe psychotic symptoms, ones that have historically been thought to be specific to schizophrenia but clearly are not," says Strakowski. "So when African-Americans present with these symptoms, the clinicians tend not to notice other kinds of signs, and they make a diagnosis of schizophrenia." (Why blacks are more likely to exhibit these behaviors isn't known; Strakowski speculates that they may receive medical care later in the course of their illness -- whatever it may be -- when its symptoms have become more florid.)
It seems clear that bias of one sort or another plays an important role in the disproportionate number of diagnoses of blacks with schizophrenia. Indeed, several large epidemiological studies, employing very careful screening procedures, found that the incidence of schizophrenia varies little among ethnic groups worldwide. But scientists haven't ruled out the possibility that African-Americans actually suffer from the illness at a higher rate, or that the illness manifests itself differently in black patients. Poor prenatal care, the stresses of poverty and discrimination and reduced access to medical services may encourage the development of the disease in those who are vulnerable, or influence its course in those who are afflicted.
More controversial still, there is some evidence that differences between blacks and whites concerning schizophrenia may have a genetic basis. In a study published last year by a consortium of universities organized by the National Institute of Mental Health (NIMH), the authors reported that some of the genes thought to predispose individuals to schizophrenia were found in different locations on African-American and European-American chromosomes. That discovery, they wrote, "lends credence to the notion that these genetic differences, together with differences in environmental exposures, may contribute to the reported differences in disease prevalence, severity, comorbidity and course that have been observed in different racial groups in the United States and elsewhere."
Still, none of these hypotheses has yielded solid answers to the question of why blacks are more frequently diagnosed with schizophrenia. "There have been concerted efforts for short periods of time to try to investigate it, but they don't seem to ever continue long enough to understand the problem," says Strakowski.
We simply don't know why it happens.
Why aren't more scientists studying the potentially dangerous relationship between race and schizophrenia? It was just this question that perplexed Richard Lewine, Ph.D., director of the schizophrenic disorders program at Emory University.
Last spring, Lewine published a survey he conducted on how schizophrenia studies handle race. His statistics were stunning: Between 1994 and 1996, under 3 percent of the articles about schizophrenia that appeared in leading psychiatric journals reported the results of race analyses. Over 83 percent failed to even note the racial breakdown of the group examined. "The empirical study of schizophrenia has been, especially during the 'decade of the brain,' the study of white men," Lewine concluded in the March issue of Schizophrenia Bulletin.
"It's as if everybody is ignoring it," Lewine marvels. That's despite a much-heralded revision of the rules under which research grants are given by the NIMH and other agencies of the National Institutes of Health (NIH). Starting in 1993, the guidelines declared, "The NIH must ensure that women and members of minorities and their subpopulations are included in all human subject research." And yet, to judge from the studies produced since then, the rule change has had very little impact -- "unless we assume that prior to the NIMH initiative, researchers paid no attention whatsoever to race," as Lewine dryly notes.
There's no doubt that there are daunting complications associated with the study of race, which is, after all, more social construction than biological fact. It's frequently difficult to assemble a sample -- matched for age, socioeconomic status and severity of illness -- that is ethnically diverse. Because the families of schizophrenics are often fractured, it's a challenge to collect information (or DNA samples) from first-degree relatives. And looking at race in our society means pulling a single strand from the tangle of other threads -- income, education, access to health care -- in which skin color is invariably enmeshed. So perhaps it shouldn't be so startling that many scientists, according to Lewine, regard race as a "nuisance variable," to be statistically controlled or factored out entirely.
But methodological complications aren't the only reasons scientists shy away from investigating race. "It is uncomfortable work," concedes Strakowski, one of the few psychiatrists who has done substantive work on schizophrenia in African-Americans. "It irritates people on all sides. No matter what you say, someone gets unhappy."
More than one researcher interviewed for this article said they'd been warned by colleagues not to invite trouble. "When I went to write this paper, a number of my mentors were saying, 'Rosemary, you've got to be very, very careful.' And I was naive enough to say, 'What do you mean? Why do I have to be careful? These are the results of my study,'" says Farmer, whose research identified differences between black and white schizophrenics. "People are afraid of being called racist. Especially in an academic environment, people are very, very sensitive about that, and they're afraid that their whole career is going to be put in jeopardy."
The silence on racial differences may also be self-imposed. "A couple of people have grabbed my arm at meetings to say, 'Well, you know, I really have found some race differences in my data, but I'll be darned if I'm going to publish them,'" says Lewine. Because it's so difficult to say anything about race without provoking a controversy, many scientists figure it's safer to say nothing at all.
There's good reason for caution, given the horrific uses to which racial comparisons have been put in the past. Mental illness was grounds for sterilization and euthanasia in the Nazi racial hygiene movement of the 1930s, as Andrew Winston, Ph.D., points out. "To Nazi physicians, comparing the frequency of mental illness in different racial groups was part of the program to insure that Germans would not be 'polluted' by the disease-ridden genes of other races," says Winston, a psychologist at the University of Guelph in Ontario who studies the illegitimate use of psychology by racist movements. And we still have to worry about that way of thinking, he emphasizes: "Contemporary racist and neo-Nazi groups are also likely to misuse research on racial differences in schizophrenia, just as they now misuse research on intelligence test scores."
Making race the focus of psychiatric research is inherently problematic, asserts Winston, "because the nature of the problem has to do with how people behave and relate to other people. That's part of the definition of whether or not you've got the disease. You have to be a lot more cautious about what the meaning of any group differences are."
But others say it's exactly this record of abuse -- and this subjectivity of clinical judgment -- that makes the scrupulous investigation of race differences so imperative in this case. If we don't know if and why schizophrenia affects blacks differently from whites, we can't determine whether they're receiving the right diagnosis and treatment. And in this regard, says Strakowski, the well-meaning neglect of racial differences is just as pernicious as the biased insistence upon them.
"Coming out of the 1970s, there was a tendency to try to treat everyone the same," he notes. "That's good in theory, but in doing so we sometimes forget or don't notice differences when they do occur." The failure to identify such genuine differences among groups -- whether they're cultural, socioeconomic or even physiological -- may leave us less able to recognize treatment that discriminates unfairly. Either way, the consequences for mentally ill minorities may be incorrect diagnoses, inappropriate treatment and the ignorance of issues that might underlie their illnesses. Our hypersensitivity to race may be doing the greatest harm to the very people it is intended to protect.
The convoluted politics of schizophrenia illustrate just how much the problem of race in this country is a problem of proportion. Our strange, single-minded obsession with skin color takes us to odd extremes: We act as though racial differences are everything, or as though they don't exist. We profess that ethnicity influences all, or that it influences nothing. In the space of a century we've traveled from the fevered fantasies of eugenicists, who sought to make race the measure of human worth, to the cautious evasions of modern scientists, who regard race as a "nuisance variable" at best and a career-wrecking quagmire at worst.
That's progress of a kind, of course -- but not the kind that helps minority-group members, the objects of all this zealous attention and studied avoidance. In a predicament rife with ironies, this one may be bitterest: Our penance for past sins is leading us to commit yet another.


Shares