Regina Rabinovich recently returned from her first trip to Africa as director of a $50 million campaign to create a vaccine against the planet's most insidious parasite. One night shortly thereafter, she woke up feverish at 2 a.m. in the Washington home she shares with her husband, a pediatrician, and three children.
"I was burning up," she recalls. "Naturally, with two doctors in the house we didn't have a thermometer, so I went to the E.R. I was 105."
The diagnosis was malaria -- the disease that had brought Rabinovich to Africa in the first place. She'd taken antimalarial pills before leaving on her tour of six villages along the Gambia River, but evidently that was not enough to prevent the mosquito-borne bug from colonizing in her bloodstream.
Rabinovich cycled through cascades of fever and shaking, burning and cold for a few days before returning home from the hospital. She had undergone her rite of passage as a malaria researcher with the Malaria Vaccine Initiative, created earlier this year by the Bill and Melinda Gates Foundation.
During the Vietnam War, in response to the more than 100,000 cases of malaria recorded among American troops, the United States invested significant funds for development of antimalarial drugs. In the decades since then, however, malaria research has been a disheartening, underfunded field -- despite the fact that the parasite is the No. 1 killer of children in Africa, claiming more than 1 million victims a year, and causes illness in 400 million people annually worldwide.
Once the U.S. military managed to control the disease among its troops, the failure of a United Nations-backed global antimalarial campaign around the same time -- stymied by stubborn mosquitoes and parasites and a lack of resources -- caused a decline in Western interest in the disease. U.S. and European governments spent less than $50 million annually on malaria research while drug-resistant strains of malaria proliferated in Africa.
Poverty and disorganization have frustrated African efforts to control malaria's spread with low-tech means -- such as spreading oil on stagnant ponds where mosquitoes breed and distributing window screens and bed nets. And until recently, few pharmaceutical companies had shown much interest in what may be the most promising solution -- a vaccine.
As it happens, though, Rabinovich may be a harbinger of a change in that picture. She was a prominent public health official at the National Institute of Allergy and Infectious Diseases before being named in December 1999 to head the private malaria initiative, part of a $1 billion philanthropic investment by the Gates Foundation for development of vaccines for the Third World. Her group plans to create partnerships with universities and private companies that commit to creating a malaria vaccine.
The Gates Foundation's spending on malaria follows upon big investments over the past few years by the National Institutes of Health, the World Health Organization and Britain's Wellcome Fund, with total spending from all sources totaling $100 million or more. What's more, the World Bank has pledged up to $500 million in interest-free loans to African countries for malaria prevention and control. And the lame-duck Congress could add to its appropriations a $1 billion tax credit program -- pushed by the Clinton administration and based on a proposal by Harvard professors Jeffrey Sachs and Michael Kremer -- to encourage spending on malaria research by the pharmaceutical industry.
Money has begun flowing into this fight for two reasons. Public health officials are worried about drug-resistant strains of the parasite that are on the rise around the world, and they are encouraged by the emergence of several promising antimalarial vaccines, which need big cash infusions to move forward.
But when both houses of Congress approved a $50 million U.S. Agency for International Development program to combat malaria on Oct. 26, another factor was at play: the self-interested inclination to do something about malaria before global climate change brings a "third-world disease" to our doorstep.
"As we know from our experience with the West Nile virus," said Rep. Barbara Lee, D-Calif., during floor debate on the bill, "if we do not act quickly to break the back of a disease abroad, the inevitable result is outbreaks of the disease here in the United States."
Global climate change does seem to be bringing more mosquito-borne diseases to this country. Scientists speculate that an errant mosquito that somehow traveled to the United States in the belly of a plane may have caused New York's 1999 outbreak of the occasionally deadly West Nile virus. By this fall the germ -- which spreads from mammals and birds to mosquitoes and back again -- had established itself all along the East Coast, prompting spraying campaigns in places as far south as the Washington suburbs. Scientists believe that the West Nile virus is here to stay, and will probably spread across the entire country within a few years.
Dengue fever, a dangerous mosquito-borne viral disease that causes joint pain and sometimes death, has dramatically increased along the U.S. side of the Mexican border in the past few years, according to research presented at a conference in Houston in November. As in the case of West Nile, dengue-carrying mosquitoes may be hitching rides across the border in tractor-trailers brought north by increased trade, with warmer temperatures allowing the virus to gain a foothold.
Malaria thrives in hot temperatures, which enable the plasmodium parasite that causes the disease to mature more quickly in the bodies of the mosquitoes that carry it. Paul Epstein, a Harvard Medical School tropical disease specialist, has presented computer models suggesting that malaria, endemic in areas of the world where 45 percent of the population lives, could affect 60 percent of the world's population by 2100 if warming trends continue.
In the 19th century, wealthy Washingtonians sent their children to cooler climes in the summer and British diplomats living in the city got hardship pay for their posting in the federal district's malarial sump. But many malaria experts are skeptical that the disease could become endemic in America again. Lifestyle changes and aggressive anti-mosquito campaigns were what rid Europe and North America of the disease, they point out, not the fact that the regions were cold.
"Yes, malaria could return to these regions," says Jo Lines, a malaria researcher in Britain, "but only if we go back to living together in unglazed houses with our animals."
Still, the return of endemic malaria in the United States is not out of the question. "If warming brought in populations of mosquitoes that are more efficient vectors than the ones we have now, it could happen," says Ripley Ballou, who led malaria vaccine research at the Walter Reed Army Institute of Research for 17 years.
In the 1930s, Anopheles gambiae mosquitoes, deadly efficient malaria carriers, were brought from Africa to Brazil by accident and caused major outbreaks before aggressive spraying campaigns subdued the invaders. The Anopheles strains of mosquitoes in this country aren't nearly as effective as Anopheles gambiae at transmitting the disease -- which may be why the United States, despite frequent cases of imported malaria such as Rabinovich's, hasn't experienced large outbreaks.
"We don't have gambiae in North America, but if they moved in because of global warming, even a small population of [these] infected mosquitoes could cause a lot more disease," Ballou says.
Still, researchers like Ballou, who retired from the military last year and now consults part time for Rabinovich's initiative, view the threat of malaria in the United States as a narrow basis for attracting funding for their work. "If we start seeing more cases of malaria in New York City and along the population centers around the country -- which is certainly possible -- there will certainly be more resources put on this," says Ballou. "But I don't see that as a very good way of moving the emphasis along."
Rabinovich agrees. Seeking increased funding based on fear would be a short-lived effort, she says, because she doubts malaria will become a chronic U.S. problem. "I'm hoping for more of a perspective that we're a global community and this is an infectious disease affecting the world, and the U.S. should have a role," she says. "That's more sustainable."
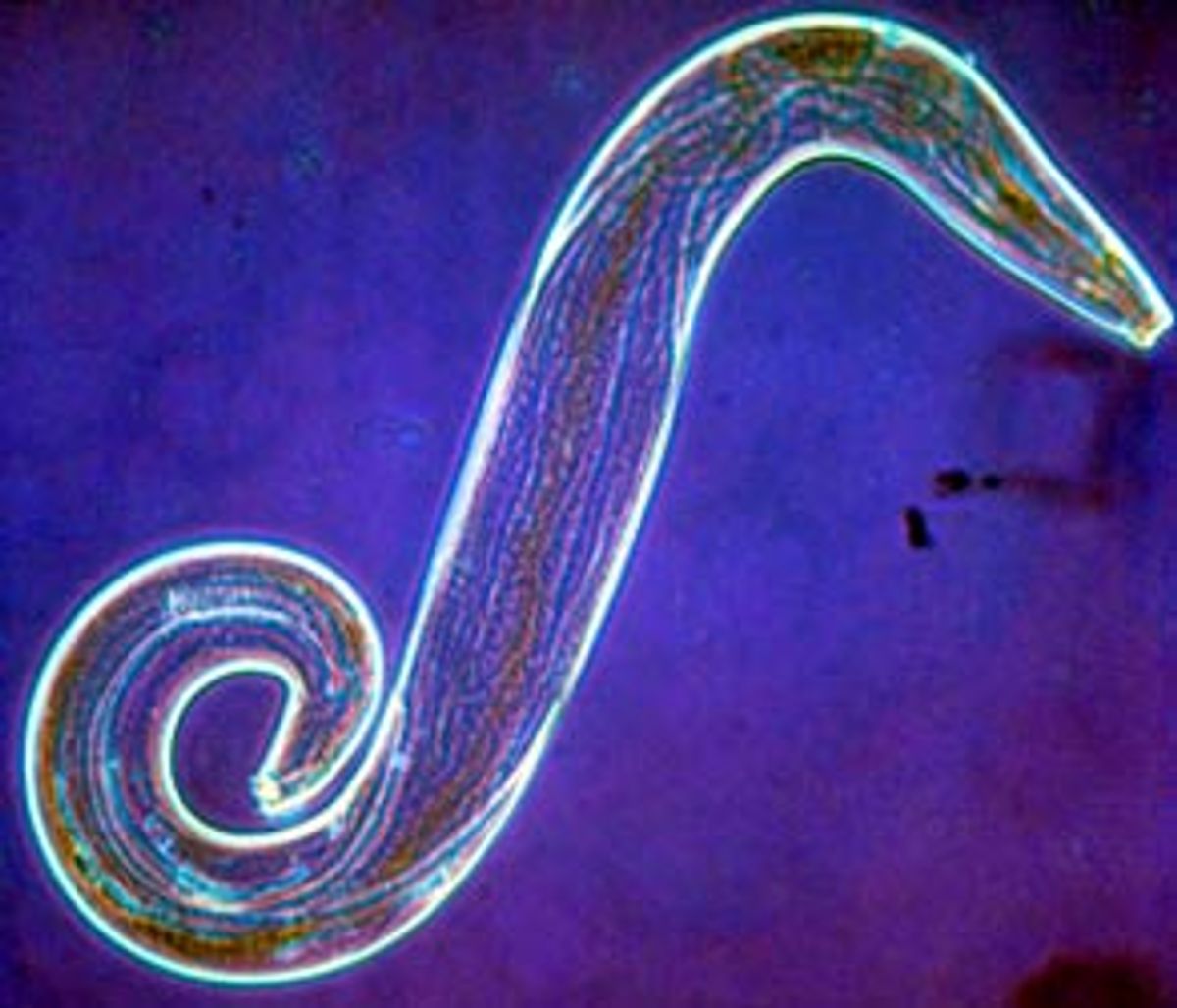
Whatever motivates funding for malaria research, there are some encouraging signs in a field with vexing difficulties. It has been tough to develop a malaria vaccine because the parasite that causes the worst symptoms, Plasmodium falciparum, has evolved a remarkable capacity to thrive in our bodies. Falciparum, the dominant strain in Africa, lives out four life stages in humans, and it tends to colonize cells in a way that protects it from a person's immune system.
Last year, for the first time, an experimental malaria vaccine successfully protected a large group of people. The trial of 306 adults was conducted in Gambia by researchers from Walter Reed; Smith Kline Beecham Biologicals (SB Bio), a Belgian subsidiary of the pharmaceutical giant; and the British Medical Research Council. The vaccinated group had 71 percent fewer episodes of malaria than the controls -- although the protection lasted only two months.
Rabinovich, whose initiative is likely to help fund further trials of this and related vaccines, was accompanying SB Bio officials on a visit to the Gambian villages that took part in the trial when she got her nasty bite.
The Gambia vaccine, known as RTS,S, marshals an immune response against malarial sporozoites, the spindly forms of the parasite that the mosquito injects into the body and that quickly swim through the bloodstream to lodge in the liver. Scientists at Walter Reed are working to incorporate another component into the vaccine so it can attack the next stage in the parasite's life cycle -- the seedlike merozoites, which propagate from the mature sporozoite and burst out of the liver into the bloodstream by the tens of thousands, colonizing and destroying an infected person's red blood cells.
One particularly awful aspect of malaria is that for reasons that aren't entirely understood, humans don't develop immunity to the disease after getting it once. "What really hits you," says Rabinovich (who during an interview in her office is wearing a sweat suit against recurring malarial chills despite Washington's October heat), "is that, OK, I've been through this. I've seen the millions of antigens multiplying in my blood, and yet the next time I go back to Africa I could get just as sick."
No malaria vaccine is likely to be as effective as, say, the measles vaccine. But in the Third World, where the parasite's resistance to common, inexpensive antimalarial drugs is growing and expensive drugs just aren't an option, a vaccine may be the best hope, as in the case of AIDS.
It would be easy to blame the drug industry for failing to develop a malaria vaccine until now. But malaria researchers make it clear that some major technical hurdles had to be crossed before sinking big bucks into a vaccine made sense.
In the United States, the only sustained, well-funded malarial vaccine work in the past few decades has been done by the military, at Walter Reed or at the Naval Medical Research Center in nearby Silver Spring, Md.
Key breakthroughs began in 1979, when scientists discovered that the sporozoite proteins could be targeted with a vaccine. From about 1986 to 1995, Walter Reed and the Navy tested nearly two dozen vaccine formulations. They all flopped.
Usually, the drill went like this: Scientists developed a new vaccine; scientists tested the vaccine on animals for safety; then the lead scientist and lab partners rolled up their sleeves, got a shot and exposed themselves to malarial mosquitoes.
Next, everyone came down with malaria.
While recovering from the disease -- whose symptoms can easily be controlled if treated quickly enough -- the scientists often learned that the company working with them on the vaccine had decided to end the partnership.
"The term 'rolling up your sleeves' has a particular connotation when it comes to malaria research," says Ballou. He got a malarial bite in 1987 while testing a failed, early-generation vaccine. Gray Heppner, now head of immunology at Walter Reed, got malaria in 1993 while testing an updated version. "That vaccine was safe, well-tolerated and completely without effect," Heppner says with a laugh. "There were 17 of us -- controls [who also exposed themselves to mosquito bites] and vaccinees -- and we all got malaria."
Companies typically worked with Walter Reed to the point of testing a vaccine on a few people. "If it didn't show results, they bailed," says Heppner. "Things were tough. An awful lot of people said it's not possible to make a malaria vaccine."
To this day, SB Bio is the only division of a major pharmaceutical company that has shown a long-term commitment to working on a malaria vaccine. A side benefit for SB Bio has been that its malaria research enabled it to test vaccine technologies with applications for other, more salable vaccines.
The military's malaria vaccine research has trundled along for years as "a flea on the back of military R&D," says Ballou. Funding for the labs was hurt some by downsizing of the military and, Ballou adds, "we didn't have a deployment where we had a lot of people getting malaria, to the point where some general hollers, 'Where's my vaccine!'" Most of the malaria drugs on the market, Ballou points out, were developed as a result of a huge drug-screening program the military funded in response to the devastating effects of malaria on U.S. troops in Vietnam.
The hope now is that private initiatives like the Gates fund -- with federal support -- can sink enough money into partnerships with researchers to lower the financial risk for the pharmaceutical companies that ultimately will have to manufacture the vaccine.
Rabinovich and other experts say that an effective, widely available vaccine is probably still at least 10 years off. In the meantime, they continue to risk their health in the hopes of saving babies. Rabinovich sometimes wears a pin with three children on it -- the number of African children who die each minute of malaria.
One night during her visit to Gambia, Rabinovich attended a celebration of the vaccine trial. Villagers performed humorous skits about the painful shots and the misery of malaria. "As dusk came down we were passing bug spray back and forth and surreptitiously rubbing it on ourselves, because you could tell what was around," she says.
For the scientists lathering themselves with protective bug juice, it was sobering to watch the children, who had no protection at all. "The village kids," Rabinovich recalls, "were all just running around."


Shares