Startled awake by the ringing of a telephone while lying in a bed in the French Quarter, a block from Bourbon Street, I found myself momentarily forgetting where I was and why I was there. Too many meetings, too many scientists. Reaching for the phone, I remembered: New Orleans. The twenty-second annual Neuropharmacology Conference — this year’s theme, “Cognitive Enhancers.” All the top “smart-pill” researchers would be there.
“This is your wakeup call,” said the automated voice on the phone.
I hung it up, lay back down, and shut my eyes. For just a moment. And then I dreamed that my head, the top of it, was expanding, like bread in an oven. My forehead grew to about twice its normal size. Just as it cracked open with a hideous noise, I saw my brains begin to bubble out.
That’s when I woke back up for the meeting.
* * *
“Why do we need cognitive enhancers?”
The second speaker of the morning was Gary S. Lynch, one of the field’s longtime leaders. He’d been among the smart-pill pioneers who, in the 1980s and 1990s, on the basis of early studies in mice and other animals, joined or started companies with futuristic sci-fi names like Cortex Pharmaceuticals and Memory Pharmaceuticals, none of which went anywhere. A lot of money had been spent, a lot of magazine articles had been written about “Viagra for the brain” and that kind of thing, but Lynch never quit his day job as a researcher at the University of California, Irvine. He’d even coauthored a book titled "Big Brain." Which, given my nightmare that morning, I found rather disturbing.
“Every four years,” he said, answering the question he had posed at the beginning of his talk, “this blight descends upon America called presidential elections. Anyone following it this year can see the need for cognitive enhancers.”
Over 250 scientists — so many that the planners of the meeting had switched it to a larger room at the Hilton New Orleans Riverside to accommodate the overflow — had come to find out if they were any closer to developing drugs that could safely enhance cognitive skills (the key word being “safely”) than they were two decades ago, when claims were first being made that success was right around the corner.
In a debate held in connection with the meeting, Nora Volkow, director of the National Institute on Drug Abuse, expressed grave worries about the drugs already on the market. Stimulants like Adderall, which are supposed to be prescribed only for attention-deficit/ hyperactivity disorder, are now used by 8 percent of U.S. high school seniors for nonmedical purposes each year, she said. A newer drug, Provigil, approved only for the treatment of narcolepsy, has also come into widespread use among students and businesspeople seeking to gain an edge. But when David Nutt, president of the British Neuroscience Association, asserted that few of those users experience adverse effects due to the drugs, Volkow shot back: “Yes, these stimulant drugs have been used by the military for more than fifty years, but what’s interesting is that the British stopped using [them] and it had to do with the fact that use of these stimulants can make a person paranoid. In the United States the use of stimulant drugs has been associated with friendly fire [due] to distortions of perceptions as well as paranoid thinking.”
Perhaps the biggest danger of stimulants like Adderall, she said, is that they can be addictive. Even Provigil has been found to be habit forming. Still, Volkow said, “If you can develop a medication that has no adverse effects and you can improve cognitive abilities either by enhancing your attention or your memory, my perspective is, why not? It would be very, very exciting that there could be such medications, [but] again I state without side effects, because the current medications that are available do have side effects.”
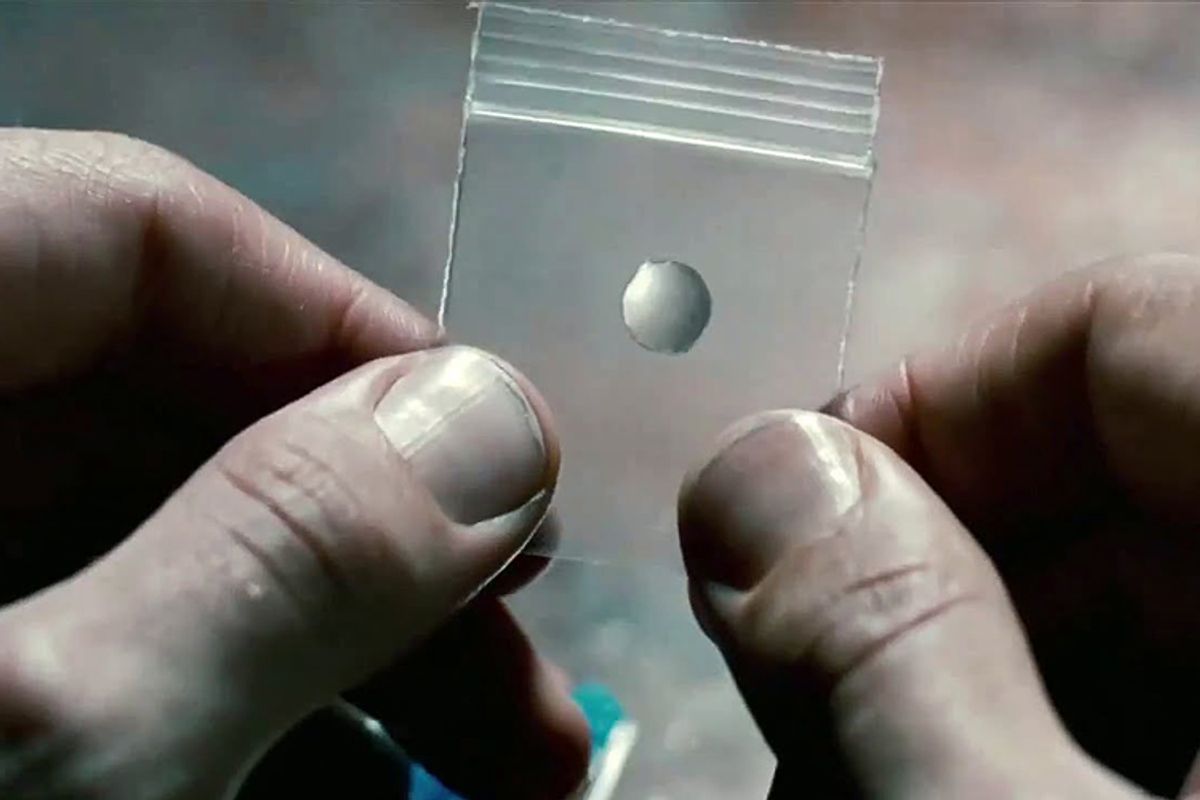
Even if currently available drugs carried no side effects, one question that students and others who use them never seem to entertain is whether they actually work — whether they truly make people smarter, better able to solve problems and remember things, or if they just keep them awake and working longer. To answer that question, Martha Farah, a psychologist at the University of Pennsylvania, presented one of the first studies ever to test thinking and learning skills in healthy, rested young people given Adderall. “The results did not reveal enhancement of any cognitive abilities,” she concluded. A trend toward a slight improvement among the lowest-performing students was seen on word recall and the Raven’s progressive matrices — but it was not large enough to be statistically significant. Despite the lack of clear benefit, Farah’s most striking finding was that participants nevertheless believed their performance was better when taking the drug than when they received the placebo. How scary is that? A pill that simply makes college students cockier.
“I want to be really clear that I’m not scolding researchers,” Farah told the group. “I’m not trying to be a nihilist or say that there’s nothing to this cognitive enhancement stuff. But the extent of our lack of knowledge is really extraordinary.”
Following her remarks, in a remarkable breach of protocol, no applause came from the audience. Farah walked from the podium in silence.
A more welcoming reception was given to Barbara Sahakian, who co-organized the meeting and who, despite holding prominent positions at both Cambridge and Oxford universities and speaking in a British accent, actually grew up in Boston. Sahakian presented encouraging results on a study she had done of thinking skills on Provigil or placebo in healthy, rested adults— one of the first such studies ever carried out. Improvements on the drug were seen, her study concluded, on “spatial working memory, planning and decision making at the most difficult levels, as well as visual pattern recognition memory following delay.” But on a test of creativity, she reported, the effects “were inconsistent and did not reach statistical significance.”
In conclusion, Sahakian said, “We need novel pharmacological treatments.” She also endorsed the use of cognitive training and other nondrug approaches to improving cognitive function. “The best effects,” she said, “might be if we combine all these treatments.”
Most of the rest of the meeting was taken up by presentations on the many dozens of new drugs now in development at universities and drug companies around the world, with names like ZIP, crebinostat, THPP-1, cytotoxic necrotizing factor 1, LSN2463359, and LSN2814617. Some were being tested against Alzheimer’s, some to restore clear thinking in people with schizophrenia or depression, and some aimed at enhancing cognition in healthy adults. Most of the new drugs had been tested so far only in mice, however, and some only in test tubes. And the presentations just kept coming.
“Fortunately we can dissolve UBP7089 in a medium which includes calcium.”
“The persistent activity of PKM zeta mediates some but not all LTM.”
“The LTP we’ve been enhancing is LTP 1. We had no idea of the existence of an LTP 2 lurking out there.”
I started looking around at my fellow attendees. Tweed jackets and bow ties, the kind still worn by scientists in movies, were nowhere to be found. To my left sat some beefy guy wearing a studded-leather wrist band. Next to him was a twenty-something with a shaved head and a camouflage-style shirt. Two rows over sat an overweight guy wearing flower-patterned Bermuda shorts and a polo shirt. A young woman beside me was puttering with her smartphone, while the guy next to her was sipping something from a tiny red bottle. I did a double take and realized it was 5-Hour Energy, the supplement containing caffeine and other ingredients, such as folic acid and vitamin B6. Seemed kind of funny that a scientist at this meeting would take such a thing. Then I saw another little bottle of it in front of the woman next to me.
And another little bottle of it was in front of me. The maker of 5-Hour Energy had somehow succeeded in placing its product at a meeting of cognitive enhancement. My attention lagging, I opened it up and drank it down. It tasted horrible. But fifteen minutes later, I did feel more alert.
And then a break was announced. Everyone started walking, and I followed, not sure where we were going. Down hallways, up stairs, we walked for over five minutes until we reached a room containing coffee and sugar cookies. Outside, on a patio, a few scientists smoked cigarettes. Between the nicotine, the caffeine, and the sugar, these researchers would stop at nothing in their quest to discover cognitive enhancers.
The most encouraging presentation of the day, oddly enough, had nothing to do with drugs. Tracey Shors, a notably cheerful psychologist from Rutgers University with long, straight blond hair, described a study she had carried out in mice. Although researchers have known for years that new neurons develop continuously in the hippocampus, a section crucial for forming new memories, little has been known about how to augment their survival. Most end up dying. So even though exercise, sex, and Prozac all help new neurons to be born, the question Shors wanted to address was how to keep them alive longer — to become a functional, permanent part of the brain. The secret, she found, was that the mice had to learn new tricks. In her experiments, she challenged them to learn how to stay on top of a rod spinning under their feet — the mouse equivalent of log rolling — while perched over a container of water.
Mice hate water.
So, highly motivated, the mice learned the footwork necessary to stay atop the rotating rod even as it spun faster. The better they got at it, the more new neurons survived in their brains.
“Tasks that are difficult to learn are the most effective,” Shors said. “If they simply exercise, they don’t retain the neurons. Learning must occur, and it must require some effort. So if you exercise, you will produce more neurons. If you do mental training you’ll keep alive more cells that you produced. And if you do both, now you have the best of both worlds, you’re making more cells and keeping more alive. The effort part is key. We need to learn things that are new, and we need to keep it challenging.”
What’s more, the cycle of neuron survival multiplies over time, she found, their numbers growing like, well, a family of well-fed mice. “Animals that learn something new at the beginning of an experiment,” she said, “several weeks later they learn a second task even faster. So brain cells that weren’t even born at the time of the first training are now more likely to survive by virtue of the fact that the older cells stayed alive. I guess the message is that if you keep learning throughout your lifetime, as more and more brain cells sursurvive, eventually your brain would explode.”
She was joking, right? I think she was joking.
Before the meeting ended, I wanted to know how long it might be before one of the new drugs being developed might actually get on the market. None of the researchers offered estimates during their presentations, so I sat down at the end of the day with one of the silver-haired lions of the field, Tim Tully. Like Gary Lynch, Tully had founded a company back in the 1990s with the goal of putting a smart pill on the market and had seen those hopes dashed. Unlike Lynch, however, in 2007 he left his day job in academia — head of neurogenetics at Cold Spring Harbor Laboratory — to become chief science officer of a new smart-pill company, Dart NeuroScience.
“I quit because when Ken Dart offered me the job, I said, ‘That’s really cool, but you have to realize it’s going to take you twenty years before you make a profit,’” Tully told me. “I thought he’d flinch, but instead he said, ‘Yeah, that’s about what I’m expecting.’ So then I was in, because I had an investor, an owner, who understood that it would take a long time and a lot of shots on goal until we’ll be successful. We scientists who once said we’d have a drug in five years, we were naïve. I now doubt that I will necessarily live long enough to see a really safe and effective cognitive enhancer in my lifetime. But I have no doubt that it will come.”
Gary Lynch, when we sat down for an interview, expressed a similar mix of caution and optimism.
“The mechanisms of this next generation of drugs being developed are well understood,” he said. “We’re seeing a lot of beautiful successes in animals. I think we’re at the point where we can see they will work in humans, if we can get past the safety bumps. But that’s a big if. The safety margins needed for cognitive enhancement are going to be very large. People are going to take these drugs repeatedly — nobody’s going to take them just once. So the winner is going to be the first one that comes through with a clean safety profile. The history of neuropsychiatry is that somewhere between the phase 2 study of a hundred people and the phase 3 study of three hundred people the beast jumps out from behind the bush: the drug turns out to have some unexpected side effect. It’s going to come down to whether or not they run into the troll under the bridge.”
As for drugs already on the market, he said he shared the perspective of most at the meeting: neither Adderall nor Provigil does much more than keep people awake and working. They might help a student finish writing a paper, but they won’t help him or her write it better. But then he mentioned another cognitive enhancer that he does consider useful, despite its nasty reputation: nicotine.
“Nicotine has a legitimate enhancing effect,” he said. “I self-medicate with it when I’m having a difficult time writing something. I’ll sit there chewing a cigar when I hit a tough spot. People say to me, ‘Do you ever take any of these drugs you’re studying?’ Nicotine, I find, helps me out.”
* * *
Back home in New Jersey, I read through dozens of human and animal studies published over the past five years showing that nicotine — freed of its noxious host, tobacco, and delivered instead by chewing gum or transdermal patch — may prove to be a weirdly, improbably effective cognitive enhancer and treatment for relieving or preventing a variety of neurological disorders, including Parkinson’s, mild cognitive impairment, ADHD, Tourette’s, and schizophrenia. Plus it has long been associated with weight loss. With few known safety risks.
Nicotine? Yes, nicotine.
In fact — and this is where the irony gets mad deep — the one purpose for which nicotine patches have proven futile is the very same one for which they are approved by the Food and Drug Administration, sold by pharmacies over the counter, bought by consumers, and covered by many state Medicaid programs: quitting smoking. In January 2012, a six-year follow-up study of 787 adults who had recently quit smoking found that those who used nicotine replacement therapy in the form of a patch, gum, inhaler, or nasal spray had the same long-term relapse rate as those who did not use the products. Heavy smokers who tried to quit without the benefit of counseling were actually twice as likely to relapse if they used a nicotine replacement product.
“I understand that smoking is bad,” said Maryka Quik, director of the Neurodegenerative Diseases Program at SRI International, a nonprofit research institute based in California’s Silicon Valley. “My father died of lung cancer. I totally get it.”
Yet for years Quik has endured the skepticism and downright hostility of many of her fellow neuroscientists as she has published some three dozen studies revealing the actions of nicotine within the mammalian brain.
“The whole problem with nicotine is that it happens to be found in cigarettes,” she told me. “People can’t disassociate the two in their mind, nicotine and smoking. It’s not the general public that annoys me, it’s the scientists. When I tell them about the studies, they should say, ‘Wow.’ But they say, ‘Oh well, that might be true, but I don’t see the point.’ It’s not even ignorance. It’s their preconceived ideas and inflexibility.”
I met Quik at the annual meeting of the Society for Neuroscience held in Washington, D.C. Amid thousands of studies presented in a cavernous exhibition hall, the title of hers jumped out: “Nicotine Reduces L-dopa-Induced Dyskinesias by Acting at β2 Nicotinic Receptors.”
“A huge literature says that smoking protects against Parkinson’s,”she said. “It started as a chance observation, which is frequently the most interesting kind.”
The first hint of nicotine’s possible benefits, I learned, came from a study published in 1966 by Harold Kahn, an epidemiologist at the National Institutes of Health. Using health-insurance data on 293,658 veterans who had served in the U.S. military between 1917 and 1940, he found the kinds of associations between smoking and mortality that even by the mid-1960s had become well known. At any given age, cigarette smokers were eleven times more likely to have died of lung cancer as were nonsmokers and twelve times more likely to have died of emphysema. Cancers of the mouth, pharynx, esophagus, larynx — blah, blah, blah. But amid the lineup of usual suspects, one oddball jumped out: Parkinson’s disease. Strangely enough, death due to the neurodegenerative disorder, marked by loss of dopamine-producing neurons in the midbrain, occurred at least three times more often in nonsmokers than in smokers.
What was it about tobacco that ravages the heart, lungs, teeth, and skin but somehow guards against a disease of the brain? Over the course of the 1970s, neuroscientists like Quik learned that the nicotine molecule fits into receptors for the neurotransmitter acetylcholine like a key into a lock. By managing to slip through doors marked “Acetylcholine Only,” nicotine revealed a special family of acetylcholine receptors hitherto unknown.
And what a family. Nicotinic receptors turn out to have the extraordinary capacity to moderate other families of receptors, quieting or amplifying their functioning. According to psychopharmacologist Paul Newhouse, director of the Center for Cognitive Medicine at Vanderbilt University School of Medicine in Nashville, “Nicotinic receptors in the brain appear to work by regulating other receptor systems. If you’re sleepy, nicotine tends to make you more alert. If you’re anxious, it tends to calm you.”
The primary neurotransmitter that nicotine nudges is dopamine, which plays an important role in modulating attention, reward-seeking behaviors, drug addictions, and movement. And therein lies the answer to the mystery of why nicotine could prevent a movement disorder like Parkinson’s disease, due to its effects on dopamine.
To put the drug to the test, Quik treated rhesus monkeys with Parkinson’s with nicotine. After eight weeks, she reported in a landmark 2007 paper in the Annals of Neurology, the monkeys had half as many tremors and tics. Even more remarkably, in monkeys already receiving L-dopa, the standard drug for Parkinson’s, nicotine reduced their dyskinesias by an additional one-third. Studies of nicotine in humans with Parkinson’s are now under way, supported by the Michael J. Fox Foundation.
Other research suggests the drug may protect against the early stages of Alzheimer’s disease. A study involving sixty-seven people with mild cognitive impairment, in which memory is slightly impaired but decision-making and other cognitive abilities remain within normal levels, found “significant nicotine-associated improvements in attention, memory, and psychomotor speed,” with excellent safety and tolerability.
“What we saw was consistent with prior studies showing that nicotinic stimulation in the short run can improve memory, attention, and speed,” said Newhouse, who led the study.
As Newhouse sees it, “Obviously the results of small studies often aren’t replicated in larger studies, but at least nicotine certainly looks safe. And we’ve seen absolutely no withdrawal symptoms. There doesn’t seem to be any abuse liability whatsoever in taking nicotine by patch in nonsmokers. That’s reassuring.”
That’s not reassuring: it’s totally bizarre. Nicotine has routinely been described in news accounts as among the most addictive substances known. As the New York Times Magazine famously put it in 1987, “nicotine is as addictive as heroin, cocaine or amphetamines, and for most people more addictive than alcohol.”
But that’s just wrong. Tobacco may well be as addictive as heroin, crack, alcohol, and Cherry Garcia combined into one giant crazy sundae. But as laboratory scientists know, getting mice or other animals hooked on nicotine all by its lonesome is dauntingly difficult. As a 2007 paper in the journal Neuropharmacology put it, “Tobacco use has one of the highest rates of addiction of any abused drug. Paradoxically, in animal models, nicotine appears to be a weak reinforcer.”
That same study, like many others, found that other ingredients in tobacco smoke are necessary to amp up nicotine’s addictiveness. Those other chemical ingredients — things like acetaldehyde, anabasine, nornicotine, anatabine, cotinine, and myosmine — help to keep people hooked on tobacco. On its own, nicotine isn’t enough.
But what about nicotine as a cognitive enhancer for people without Alzheimer’s, Parkinson’s or any other brain disease?
“To my knowledge, nicotine is the most reliable cognitive enhancer that we currently have, bizarrely,” said Jennifer Rusted, professor of experimental psychology at Sussex University in Britain when we spoke. “The cognitive-enhancing effects of nicotine in a normal population are more robust than you get with any other agent. With Provigil, for instance, the evidence for cognitive benefits is nowhere near as strong as it is for nicotine.”
In the past six years, researchers from Spain, Germany, Switzerland, and Denmark — not to mention Paul Newhouse in Vermont — have published over a dozen studies showing that in animals and humans alike, nicotine administration temporarily improves visual attention and working memory. In Britain, Rusted has published a series of studies showing that nicotine increases something called prospective memory, the ability to remember and implement a prior intention. When your mother asks you to pick up a jar of pickles while you’re at the grocery store, she’s saddling you with a prospective memory challenge.
“We’ve demonstrated that you can get an effect from nicotine on prospective memory,” Rusted said. “It’s a small effect, maybe a 15 percent improvement. It’s not something that’s going to have a massive impact in a healthy young individual. But we think it’s doing it by allowing you to redeploy your attention more rapidly, switching from an ongoing task to the target. It’s a matter of cognitive control, shutting out irrelevant stimuli and improving your attention on what’s relevant.”
Of course, all the physicians and neuroscientists I interviewed were unanimous in discouraging people from using a nicotine patch for anything other than its FDA-approved purpose, as an aid to quit smoking, until large studies involving hundreds of people establish the true range of benefits and risks (even though studies find it doesn’t work for that purpose). But with so many studies showing that it’s safe, and so many suggesting it might well be the most effective cognitive enhancer now on the market, I decided to ignore not only their advice but the advice of my personal physician.
I added a nicotine patch to my list.
* * *
Thumb-tacked to a cubicle wall outside the office of Roy Hoshi Hamilton, director of the University of Pennsylvania’s Laboratory for Cognition and Neural Stimulation (LCNS), is a photo-manipulated advertisement for Dos Equis. It shows the suave, gray-haired, bearded actor who portrays the Most Interesting Man in the World sitting next to his usual bottle of beer. Over the Dos Equis label, however, another label had been substituted, showing a brain with bolts of electricity surrounding it. The tagline of the campaign has also been altered. “I don’t always non-invasively stimulate my brain,” it states, “but when I do . . . it’s at the LCNS. Stimulate responsibly, my friends.”
It turns out there is a safer and more reliable way to stimulate your brain than with beer, whiskey, coffee, Adderall, Provigil, or any other known drug, whether approved or in development. With surprisingly little public attention, given its stunning successes in randomized clinical trials, the field of noninvasive brain stimulation has produced results that seem straight out of science fiction. Using voltages so low they can be generated with the same 9-volt batteries that power a flashlight, transcranial direct-current stimulation, or tDCS, causes neither convulsions nor almost any other known side effect beyond a mild tingling when current is applied to the skull. The procedure takes just twenty minutes, repeated for a mere five to ten days. Yet studies published in leading scientific journals since 2005 have shown that tDCS can improve outcomes for a variety of purposes that include (deep breath) depression, stroke, traumatic brain injury, long-term memory, math calculations, reading ability, complex verbal thought, planning, visual memory, the ability to categorize, the capacity for insight, and the solving of an inherently difficult problem.
Too good to be true, right? How can a minuscule amount of electricity, applied to the skull for twenty minutes with the same kinds of positive and negative cables used to jump a car battery, make people think better?
When I posed that question to Hamilton in his office on the fifth floor of the university’s Goddard Laboratories building, he leaned back in his chair, smiled, and answered, in the classical style of an ancient philosopher, with his own question.
“What is a thought? A thought is what happens when some pattern of firing of neurons has happened in your brain. So if you have a technology that makes it ever so slightly easier for lots and lots of these neurons, these fundamental building blocks of cognition, to be active, to do their thing, then it doesn’t seem so far-fetched that such a technology, be it ever so humble, would have an effect on cognition. How could it affect it enduringly? There’s this mantra in neuroscience, coined by Donald Hebb: Neurons that fire together wire together. So I have this tool that makes it more likely your neurons will fire. Now, while I’m applying the current I’m going to have you engage in some behavior, a working-memory task, say, or reading aloud some words even though you have aphasia following a stroke, which is my area of interest. So now that network of neurons is being activated in an environment that slightly nudges it, makes it slightly easier for the neurons to fire and the behaviors to be successfully carried out. Then it’s not too far-fetched that, when that happens over and over again, during two weeks of practice, those pathways will be reinforced. I agree it does seem very simple. It’s not, we’re inserting some super-high-tech nanorobots into your brain to clear up your carotid arteries. But it is in accord with our thinking about how brains work. And it does appear to have wide-ranging effects.”
With a brown goatee, curly salt-and-pepper hair, and tawny skin that could pass for Italian or Hispanic, Hamilton is actually Japanese-African-American. “Hoshi, my middle name, is my mother’s maiden name,” he told me. “She’s from the Fukushima area. And my father’s from Oakland. They met in Los Angeles. My mother came to the United States in the hopes of advancing her English studies. That plan was altered. She and my father got married. I grew up in Long Beach, approximately twenty-seven miles south of L.A.”
After graduating magna cum laude from Harvard with a BA in psychology, Hamilton planned to become a psychiatrist. But in his first year at Harvard Medical School, he explained, “I went to a lecture by the behavioral neurologist Alvaro Pascual-Leone. He had just arrived at Harvard as a new assistant professor. He was talking about how blind individuals could perform these remarkable tactile tasks, touch-related tasks, and when they did so, they activated parts of their brain that you and I would use for vision. They’re activating their visual cortex when they’re touching stuff. Alvaro demonstrated that he could manipulate that by placing a powerful magnet to the back of the blind person’s head, zapping that region of the brain. In that instant, their ability to perform those remarkable tactile tasks is reduced. He demonstrated that you can use a piece of technology to manipulate brain activity in a focal, precise way. I thought, ‘That’s the coolest thing I’ve ever seen in my life and that’s what I’m going to do.’ ”
That was in the mid-1990s, when Pascual-Leone was pioneering the use of transcranial magnetic stimulation to explore and manipulate the function of brain regions. Hamilton ended up taking three years off from his medical school education to work in Pascual-Leone’s laboratory before finally obtaining his Harvard medical degree, cum laude, and then completing his residency in neurology at the University of Pennsylvania, where he is now an assistant professor. Hamilton has now published ten studies in a span of three years demonstrating that tDCS can help adults with dyslexia to read better and can improve the ability of stroke patients suffering from aphasia to find the words they’re searching for.
But all those studies lasted only ten sessions. Three miles to the northwest of Hamilton’s lab, on the campus of Temple University, neuroscientist Ingrid Olson was conducting a study giving tDCS for thirty days in a row to college students.
“Short-term, it’s super safe,” she told me. “There have never been any serious adverse effects reported. But we don’t know the consequences of getting it for thirty days in a row. It’s possible you could make yourself really good at working-memory tasks but that, in doing so, you might get worse at something else.”
One reason she and other researchers have been interested in tDCS is that the devices are portable and relatively inexpensive, costing as little as a few hundred dollars. Physicist Allan Snyder of the University of Sydney in Australia has even referred to the devices as a kind of “thinking cap.” But the low cost — and the fact that similar devices, approved by the FDA for treating muscle pain, are already on the market — is causing worries for Olson and her fellow sober-minded academics. Videos have already begun to appear on YouTube showing young men experimenting on their own brains with homemade tDCS devices, looking for all the world like they’re competing to join the cast of "Jackass." When applied by scientists like Olson, the positive and negative cables are carefully placed on the skull over the particular brain areas they seek to modify.
“If you put a stimulator on the back of your head,” she said, “you could stimulate your brain stem. You don’t want to mess with your brain stem.”
Olson has already published studies showing that tDCS given for ten days improves memory for the names of people whose fame is past its peak — actors like Barbara Eden, of the 1960s television show "I Dream of Jeannie," and politicians like Tony Blair, the former prime minister of England. She has also shown that it can improve verbal working memory. When training on a working-memory task for ten sessions over two weeks, the participants who received active tDCS improved twice as much as those who received a placebo version, in which the electricity is turned on initially but then slowly turned off.
“We all have limited time and stamina,” she told me. “If you could get the same gains in half the time, wouldn’t you want that? Everybody would.”
When I said I was hoping to get treated with tDCS as part of my training regimen, Olson said she would need to go through a great deal of bureaucratic wrangling to get her university to allow her to treat me. “We have lots of restrictions,” she said. But, she added, “I would not worry about having a relative of mine do it. My husband told me last night that if we keep finding benefits, he wants to be in one of our studies, because he feels like his memory is getting worse.”
I explained that I wanted to add tDCS to a regimen including physical exercise, N-back training, meditation, and other interventions.
“That’s kind of neat,” she said. “We talked in my lab about doing a study like that. We said, why don’t we just do this megastudy, where we combine every intervention we know of to improve cognitive abilities, and see what the additive effects would be.”
What did she think the effects would be?
“The fact is, nobody knows,” Olson said. “If anyone tells you they know, they’re bullshitting you.”
I added tDCS to my list.
And that was the last of the seven activities and treatments for which I found credible scientific evidence that they could increase fluid intelligence, along with N-back, Lumosity, physical exercise, mindfulness meditation, learning a musical instrument, and wearing a nicotine patch. But now I had something else to figure out: how to actually put these into practice in my daily life.
Excerpted from "Smarter: The New Science of Building Brain Power" by Dan Hurley. Copyright © 2013, Penguin. All rights reserved.


Shares