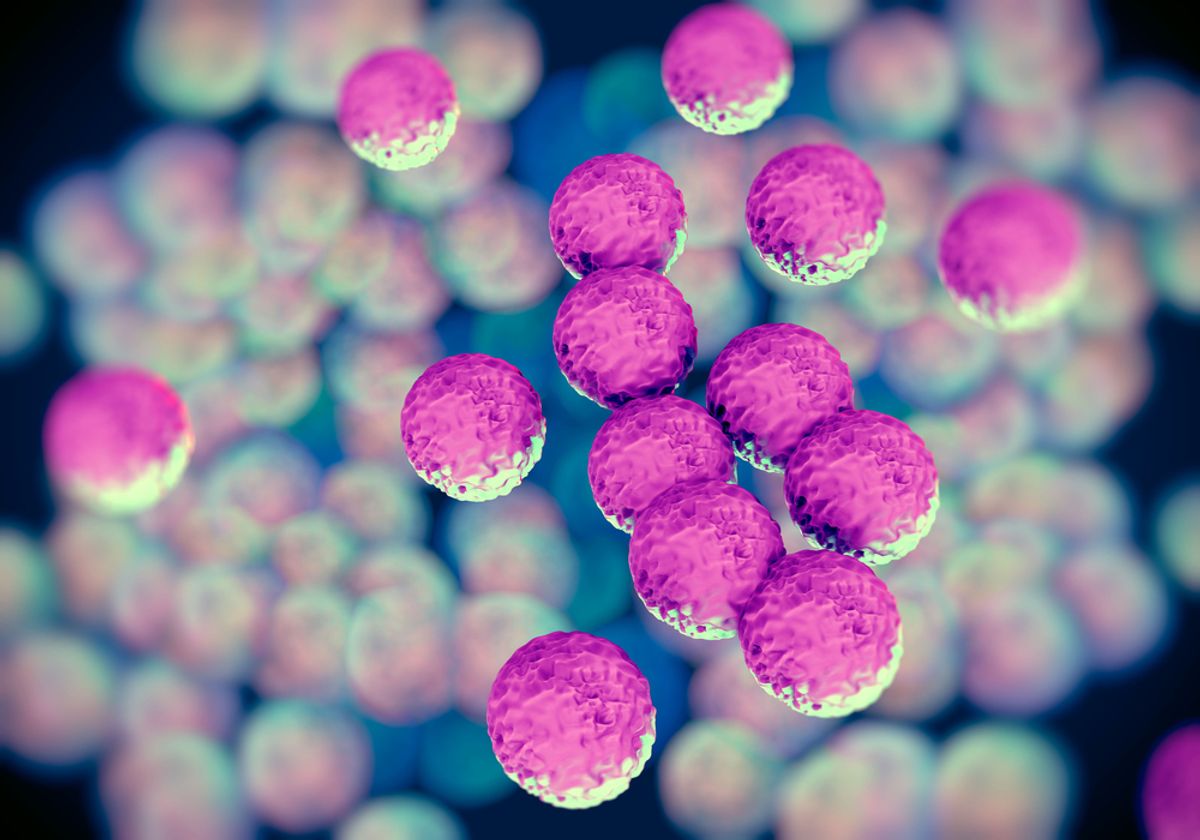
Avoiding hospitals, gyms and communal showers isn't a failsafe against getting infected with MRSA -- that's methicillin-resistant Staphylococcus aureus -- a new study in the Proceedings of the National Academy of Sciences suggests. Instead, researchers tracing a specific strain of the contagious staph infection found that the bacteria has also been breeding in private households, meaning that homes play a "critical role as reservoirs for transmission."
Nature has the scoop:
Researchers examined the prevalence of the USA300 strain in northern Manhattan and the Bronx, where it has caused an epidemic of skin and soft-tissue infections in recent years. In 2009, it was responsible for around 75% of community-acquired MRSA infections in northern Manhattan.
Anne-Catrin Uhlemann, a microbiologist at Columbia University Medical Center in New York, and her colleagues sequenced the genomes of 400 samples of MRSA collected from 161 people between 2009 and 2011, and compared them with samples from healthy people (many healthy people carry S. aureus bacteria, which could be MRSA). They also gathered data on study participants' medical histories, antibiotic use and home locations to identify a network of USA300 transmission.
...Samples from people in a single household tended to be more similar to each other than to samples from other households, which implies that individuals within a home frequently exchange S. aureus. But people were also getting infected outside the home: “There were some households where we found multiple kinds of USA300, which is quite surprising,” says Uhlemann. “It suggests some kind of outside reservoir, such as a link to a hospital or a gym.” It seems that the USA300 strain spread in public spaces first, but it is now prevalent in households as well as hospitals. Further studies are needed to evaluate how hospitals might be involved in spreading the bacteria back into the community, say the study authors.
Aside from the disconcerting implication that nowhere is safe, the researchers noted that nearly two-thirds of their samples were fully or partially resistant to routinely prescribed antibiotics -- making yet another strong case for taking the overuse of antibiotics seriously. As Uhlemann put it: "We have to limit our antibiotic use because the consequences may really be a lot of collateral damage."


Shares