In November, the World Health Organization declared that Zika was no longer a public health emergency of international concern.
That doesn’t mean concern over Zika is over, but now that a link between Zika and microcephaly has been established, it is viewed as a long-term problem, which requires constant attention.
While researchers have concluded that Zika infection can cause microcephaly and other birth defects such as eye damage in newborns, there are still many unanswered questions about the virus.
Earlier Zika outbreaks in Africa and Asia were gradual, continuous and associated with mild clinical outcomes, but the Zika outbreaks in the Pacific in 2013 and 2014 and the Americas in 2015 and 2016 have been explosive. They have been associated with severe disease, including birth defects in newborns and Guillain-Barre, a condition that can cause temporary paralysis in adults. Scientists are trying to figure out why.
I study flaviviruses, which include Zika and dengue, at Florida Gulf Coast University. Like other flavivirus researchers, I am turning to dengue to better understand Zika. Dengue, a close relative of Zika, is regularly found in places like Brazil, and is spread by the same mosquitoes, Aedes aegypti.
My colleagues and I wanted to find out whether having immunity to dengue from an earlier infection could make a Zika infection worse.
A brief history of Zika
Zika was first isolated in Uganda in 1947. For decades Zika infections in humans were sporadic. Perhaps cases of Zika went underreported, since its symptoms were similar to other fever-causing diseases and most cases are asymptomatic.
By the 1980s, Zika had spread beyond Africa and had become endemic, or habitually present, in Asia. Many individuals living in these regions may be immune to the virus.
The first reported Zika outbreak outside of Africa and Asia occurred in the Pacific, in Micronesia, in 2007. To our knowledge there were no associations with microcephaly or Guillain-Barre reported at the time.
Zika transmission in the Pacific wasn’t reported again until 2013, when French Polynesia experienced an explosive outbreak. In 2014 further outbreaks were reported in New Caledonia, Easter Island and the Cook Islands. When French Polynesia experienced another outbreak in 2014, there were reports of Zika being transmitted to babies, most likely in utero, and complications associated with Guillian-Barre in adults.
By early 2015 the virus had spread to the Americas, and the first confirmed case of locally acquired Zika in the region was confirmed in May 2015 by Brazil’s National Reference Laboratory. The Pan American Health Organization reports that Zika virus transmission had occurred in over 48 countries or territories in the Americas, with 177,614 confirmed cases of locally acquired Zika in the region, over half a million suspected cases, and 2,525 confirmed congenital syndrome associated cases with Zika infections as of Dec. 29.
Why did Zika start to cause explosive outbreaks? And why did it start to cause more health problems?
Dengue a common connector
A few factors might explain. For instance, perhaps the difference may lie in the age of the person exposed to Zika.
If children are infected before they reach puberty, they become immune and cannot pass Zika along to their children. And in parts of the world where Zika is endemic, people are more likely to have been exposed and become immune while young.
The scenario we’ve seen in the Americas is different. Since Zika had not been reported in the region prior to 2015, people, including women of child-bearing age, had never been exposed to the virus. However, this doesn’t explain why certain people develop severe disease, whereas others do not.
Dengue virus is endemic many parts of Asia, Africa and the Americas, infecting up to 100 million people globally each year. And the areas of the Pacific and the Americas that experienced explosive Zika outbreaks have two things in common: they had not been exposed to Zika before and dengue is endemic. And dengue may provide a clue to why Zika has caused severe disease in these new outbreaks.
Could a prior dengue infection make Zika worse?
When a person is infected with a particular virus for the first time, the immune system springs into action, producing antibodies to destroy it. The next time a person encounters that virus, the body produces those antibodies again to fight back, preventing illness. This is called immunity.
There are four different kinds of dengue virus, called serotypes. Antibodies produced during infection with one dengue serotype confer lifelong immunity against only that particular serotype. If a person is infected with another serotype later on, the antibodies from the earlier infection will bind to the new virus type, but can’t prevent it from infecting cells.
Instead, the bound antibodies can transport the viruses to immune cells that are normally not infected by dengue. In other words, if a person is infected with one serotype of dengue and then gets infected with another serotype, the antibodies from the previous infection then make the new serotype infect cells that it otherwise wouldn’t. Then the virus can reproduce to very high numbers in these cells, leading to severe disease. This process is called antibody-dependent enhancement, or ADE.
Zika virus is closely related to dengue and has been shown to undergo ADE in response to other flavivirus antibodies. Zika virus antibodies in turn have been shown to have a similar effect on related viruses. And other researchers have shown that preexisting immunity to Zika can enhance dengue virus disease severity in animals.
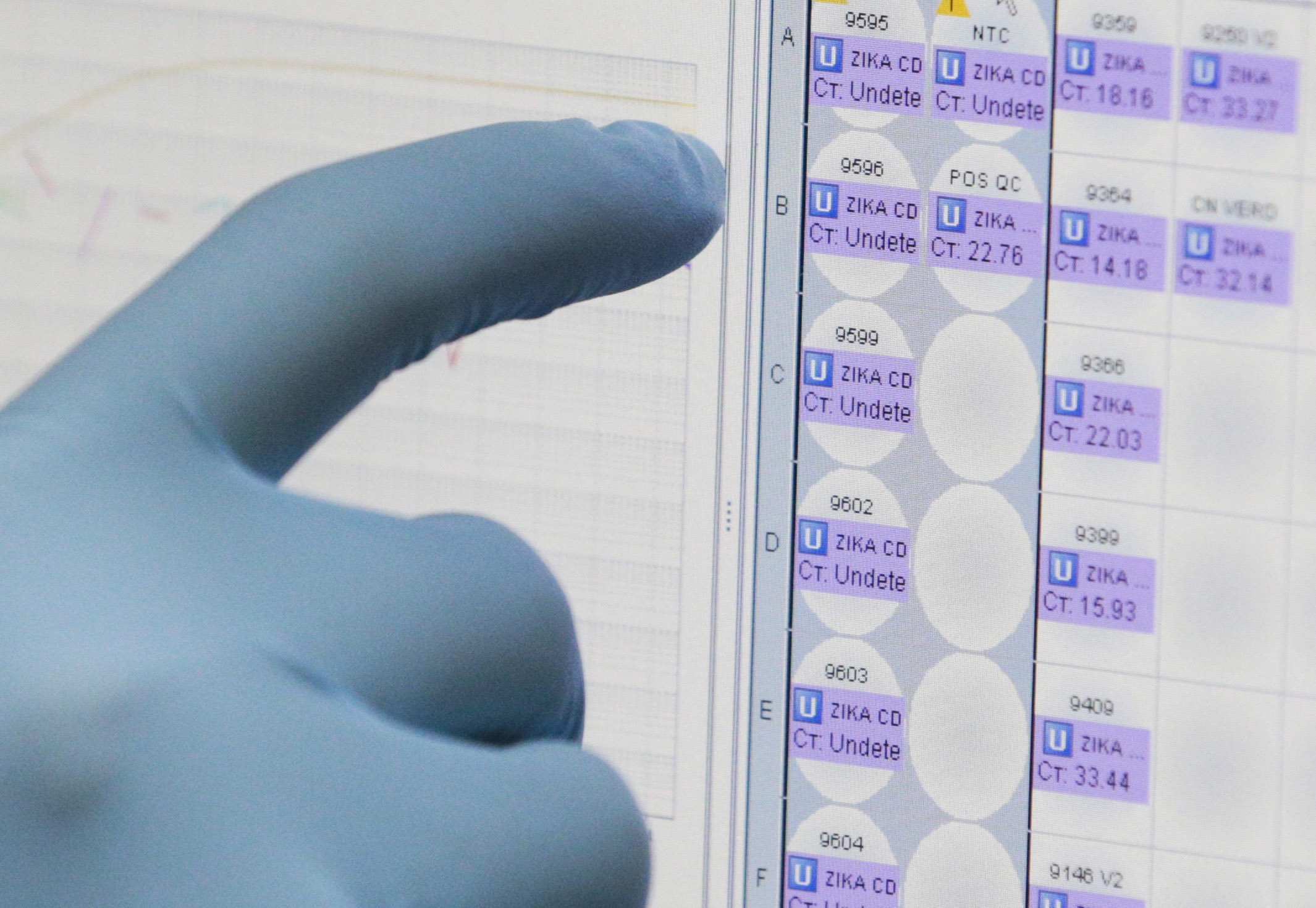
My lab studied the African strain of the Zika virus in 2015 before the connection with microcephaly was known.
Our results, posted in April to bioRxiv, a preprint server for biology, showed that antibodies from a prior dengue virus infection greatly enhanced Zika virus production in cell culture. Other groups have since independently verified our work. And, as we found in a more recent study, the same results hold true with a strain of Zika isolated in Puerto Rico by the CDC.
Our findings suggest that preexisting dengue virus antibodies may enhance Zika virus infection in patients, potentially making the infection more severe.
However, this correlation needs to be confirmed in the clinic. We do not know how many people infected with Zika in the outbreaks in the Pacific and in the Americas had prior dengue infections. But since the virus is endemic in those areas, it is possible that some people may have been infected with dengue before they were infected with Zika.
Zika’s spread may become limited
Like dengue and other mosquito-borne viruses, Zika spread is seasonal, and outbreaks occur when mosquitoes are abundant. As the United States heads into winter and South America heads into summer, what can we expect with regard to Zika and dengue and disease severity?
As more and more people acquire immunity to Zika, its spread will be limited to those who have never been exposed. Given enough time, new infections will be limited to the young. As long as infections occur prior to child-bearing years, microcephaly in newborns should not be a concern.
If these studies hold true in the clinic, cocirculation of Zika and dengue could increase the severity of both viruses. Vaccines to protect against Zika, and dengue for that matter, would need to be designed carefully so that vaccination with one does not enhance a natural infection with the other virus.
Public health emergency or not, there is still much to be learned about Zika virus and its associated consequences.
![]()
Sharon Isern, Professor of Biological Sciences, Florida Gulf Coast University