The late NFL tight end Konrad Reuland and baseball Hall of Famer Rod Carew became forever linked when Carew, who needed a new heart, received Reuland’s. Reuland suffered a brain aneurysm on Nov. 26, 2016 and died two weeks later. Medical experts and sports historians believed it to be the first heart transplant operation between two major league athletes, and the story of Reuland’s gift and Carew’s recovery touched the hearts of fans across the country.
Reuland’s decision just a few months earlier, as a 20-something who appeared to be the very picture of health, to check the organ-donor box on a driver’s license form, changed not only the course of Carew’s life but those of two other people who received Reuland’s liver and kidney. Carew, who played for the Minnesota Twins and California Angels and ended his career with 3,053 hits, received the other kidney. Carew had suffered a major heart attack in 2015 and had been placed on a waiting list for a heart transplant.
Carew, whose jersey number was 29, did not know at the time of his surgery on Dec. 16, 2016 that he was receiving Reuland’s heart, and Reuland’s family did not know who the recipients of the 29-year-old’s organs would be. Reuland died Dec. 12, 2016.
But Mary Reuland, Konrad’s mother, figured out the connection between Carew and her son a few weeks later. She had read about the lifesaving heart transplant that Carew received four days after Konrad’s death, and several people had asked her if she thought Carew could have been the recipient. Curious, Mary Reuland called the organ donation network, which matched Konrad’s heart to Carew. She learned that her son’s heart was in fact the one that saved Carew’s life. The families met less than three months later, and Mary Reuland listened with a stethoscope to her son’s beating heart inside Carew’s chest.

AP Photo/Chris Carlson
As a medical professional and sports fan, I was deeply moved by these events. But as a neurosurgeon who specializes in brain aneurysm, I was deeply pained at the news of how Reuland lost his life: Reuland suffered a ruptured brain aneurysm after lifting weights. He had been with his family for Thanksgiving, and they were decorating their home for Christmas. Reuland didn’t live to see the holiday. He had brain surgery in late November to try to repair the burst aneurysm. Just two weeks later, he succumbed in a way all too familiar to me.
There is no evidence that brain aneurysm is related to traumatic brain injury. So how is it, many may wonder, that a young athlete in phenomenal shape could suddenly develop a deadly condition?
From out of the blue
An aneurysm is a weak spot on the wall of an artery.
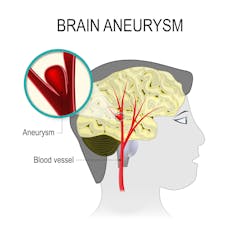
An aneurysm occurs in a weak spot in the wall of an artery. Sometimes, that weak spot expands, almost like a water balloon.
Designua/Shutterstock.com
The Brain Aneurysm Foundation estimates that 6 million people, or one in 50, have an unruptured brain aneurysm. Aneurysms can be detected by imaging, but screening imaging is not recommended unless there are symptoms or there is a strong family history of brain aneurysms. Over time, the weak spot expands almost like a water balloon. If it keeps expanding, it will eventually reach a breaking point and burst. The causes are largely unknown. Some may be hereditary.
Aneurysms can form anywhere in the body, but brain aneurysms occur in the blood vessels of the brain, usually at the base. Aneurysms tend to form at branching points where blood vessels diverge.
Brain aneurysms affect young and old, rich and poor, those with a family history of aneurysms and those without.
They typically strike without warning, and 50 percent of the time prove fatal, throwing families into shock and sudden grief. Four out of five people who suffer a brain aneurysm have no family history of it. There is some indication in the research that smoking puts you at higher risk, and that aneurysms disproportionately affect women.
But no one knows for sure what causes brain aneurysms, which affect up to 5 percent of Americans and result in 30,000 cases of ruptured aneurysms each year.
Symptoms of a brain aneurysm include headaches, double vision, vision changes, seizures or other neurological changes.
The real problem occurs when the aneurysm ruptures.
Patients with a ruptured aneurysm experience bleeding in the brain called subarachnoid hemorrhage, which is a type of stroke. Such patients may feel an overpowering “thunderclap” headache. They may die suddenly or be found comatose. When a patient has a ruptured aneurysm, we try to treat it so that it doesn’t rupture again. If it ruptures a second time, there is an 80 percent chance of death.
A devastating disorder
The statistics for this devastating disorder are grim: When a brain aneurysm ruptures, there is a 15 percent chance of death before even getting to a hospital. Of those who survive, there is a 30 to 50 percent chance of permanent disability, ranging from severe brain damage to more mild cognitive difficulties. Many are unable to return to work.
Current research in the field of cerebral aneurysm points to inflammation as a possible cause for aneurysms to arise. Here at the University of Florida, my laboratory is investigating the role inflammation may play in the development of aneurysms.
My laboratory is studying how the dynamics of blood hitting those blood vessel branching points at the base of the brain can cause inflammation. We are examining how inflammation causes weakening of a blood vessel, which we believe causes the aneurysm to develop.
We are also studying different types of inflammatory cells that cause aneurysms to rupture, so that we may work toward a goal of developing a drug treatment to fight those inflammatory cells. We are studying cytokines, or molecules that send signals, control the activities of cells and recruit those inflammatory cells to the weak part of the blood vessel. We are investigating ways to treat aneurysms by turning inflammation on or off.
While my team vigorously pursues that work in the lab, here is what I see at the hospital: patients who come in with “the worst headache of my life” – who literally had no foreshadowing of what was to come. In those cases, the aneurysm may have already ruptured.
Patients diagnosed with an unruptured aneurysm often learn of it incidentally. Maybe they came in for double vision or headaches. Maybe it was cranial nerve palsy, or, in rare cases, a seizure.
Patients with an aneurysm may undergo surgery. This involves opening the skull and pinching off the aneurysm with a metal clip. Or they may receive endovascular treatment, in which I thread a small tube through an artery in the leg all the way up to the brain to fill the inside of the aneurysm with soft packing wires called coils or place a stent, a metal mesh tube.
Every day, I see the devastating consequences of this mysterious and tragic condition.
It not only affects individuals. It affects families. It affects communities.
My goal is to identify the cause – and to pursue preventative and therapeutic treatments.
Brian Hoh, M.D., Professor of Neurosurgery, University of Florida



Shares