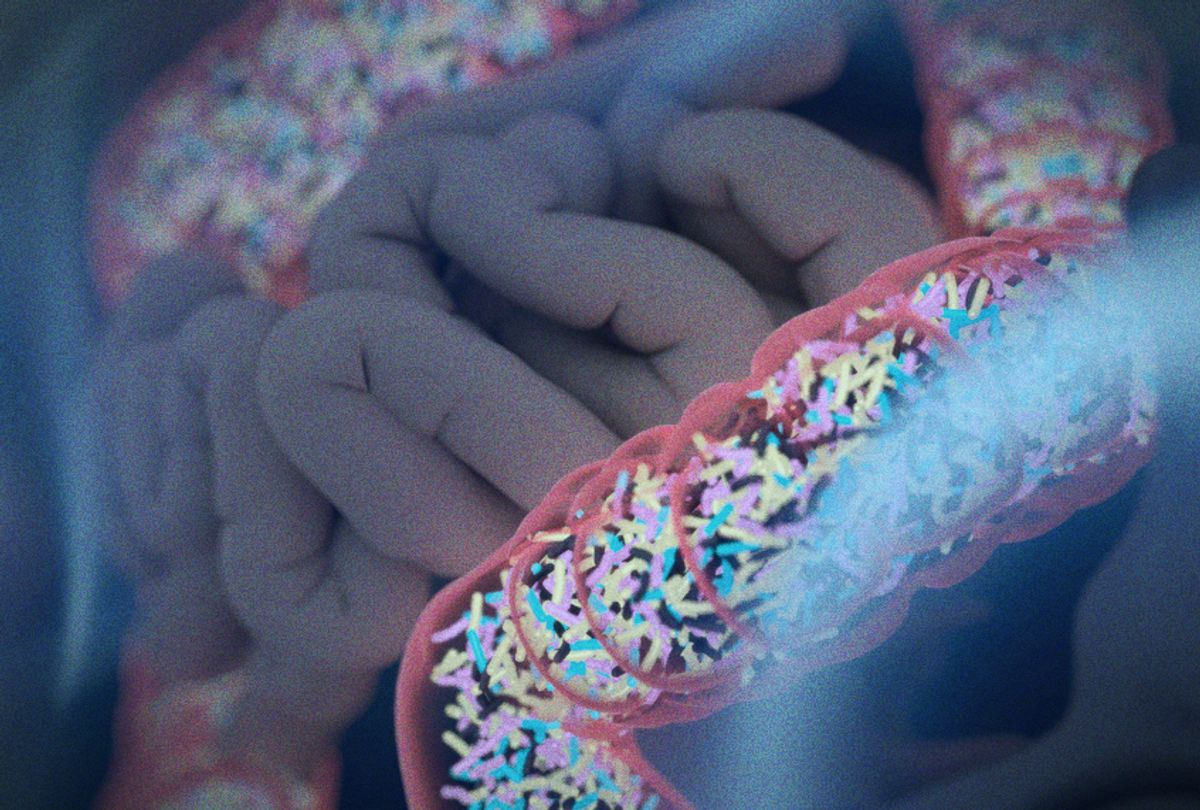
Without getting ahead of ourselves, we can start by noting that the key to staying healthy and free of inflammation and chronic illness is a well-functioning intestinal flora. Simply put, this flora is the bacteria and microorganisms that exist naturally in the intestine. In an adult, this is between 3.3 to 4.4 lb of bacteria. The intestine is a huge ecosystem containing several hundred different types of good and bad bacteria, which is an amount at least ten times greater than the number of body cells we have—approximately a hundred trillion. So, in that respect, you’re actually more bacteria than human. Most of your immune defense (or immune system, as it is also called) is in the gut (gastrointestinal tract), a truly fascinating system that’s built on a close collaboration between immune cells in the intestinal wall and your army of good intestinal bacteria. To fight inflammation, it is vital that only the good bacteria hook onto those immune cell receptors in the intestine. If the bad bacteria latch on to the receptors instead, you will have inflammation and lesser resistance against infection.
Even though the atmosphere in the gut is so influential to how we feel, it is still one of the most unchartered areas of our body. You might think it’s a bit odd when you realize that 70 to 80 percent of our immune system is situated there. But in recent years, interest in gut and intestinal flora has positively skyrocketed. Scientific research shows that bacteria in the colon not only affects a long list of illnesses and other conditions, such as diabetes, allergies, asthma, MS (multiple sclerosis), autism, cardiovascular disease, and some cancers, but also that they communicate with the brain and can drive our body weight, personality, and even our behavior. There are far more links between our gut and our brain than we first knew, with some scientists going so far as to call the gastrointestinal tract “our second brain.”
For example, it isn’t simply too little exercise and too much food that makes us fat: research shows that obesity can just as often be caused by inefficient gut flora and inflammation. Some studies even suggest that intestinal bacteria can influence our feelings of hunger and push us to crave certain foods that make their specific strain stronger than other bacterial strains in the gut. Studies have been set up where slim subjects were given intestinal flora from overweight donors, the outcome being that the slim subjects became overweight. This demonstrates that bacteria can sway us and make us fat by tricking the brain into believing that we’re hungry.
Another thing we found very interesting is the connection between intestinal flora and depression. Your risk of being diagnosed with clinical depression increases substantially if you suffer from chronic inflammation. By now it hasn’t escaped anyone’s notice that exhibiting a low level of the neurotransmitter serotonin is linked to depression and dejection. These days, the amount of prescriptions written for serotonin-boosting antidepressants (SSRI, Selective Serotonin Reuptake Inhibitors) is astronomical. Approximately more than one in ten Americans take antidepressants, and the rate at which those prescriptions are issued is rising faster still for young people and teenagers. Naturally, we were surprised to learn that only 5 to 10 percent of serotonin is found in the brain. Where is the remaining 95 percent hiding out? Answer: in the gastrointestinal tract. By the way, serotonin is not the only hormone made in the gut; intestinal flora is in fact a key player in the production of all the body’s hormones, providing our organs with these very important substances.
We could go on about this, but we do have to end it somewhere. All these findings are overwhelming; it’s even more head-spinning to realize that it wasn’t that long ago when medical students and budding dieticians were taught that bacteria in the body didn’t play an important function. Today, vigorous research is being conducted in that field, and new studies are continually proving how critical our intestinal flora is to both our physical and mental well-being.
There is an all-out war in your gastrointestinal tract
Almost one hundred years ago, the Danish scientist Christian Gram discovered that some bacteria absorbed color through their cell walls while others didn’t. Since then, bacteria that soak up color have been called Gram-positive (Gram+), while the nonabsorbent bacteria are called Gram-negative (Gram-). Plainly put, Gram+ are bacteria that protect against illness, while Gram- are the nasty ones, bacteria that, among other things, produce the strongly inflammatory and disease-inducing endotoxin poison. Since almost all Gram+ bacteria are benign and most of the Gram- are detrimental to our health, we thought we would keep things simple by referring to Gram+ and Gram- as good and bad bacteria.
When we are at our peak, we have about a hundred billion (and a thousand different strains of) good bacteria in our gut that work full-time to extract beneficial substances for us. Ideally, there should be about one nasty bacteria per one million (1,000,000) beneficial ones, but with today’s nutritional habits we are nowhere near this ratio. We are correct in asserting that there is war in our gastrointestinal tract—a conflict between our good Luke Skywalkers and evil Darth Vaders.
You can trust your good Luke Skywalkers—they’re always ready to defend your health, so long as you give them the right fuel. When you eat raw vegetables, they start multiplying rapidly and form an army so big and powerful that it can swiftly beat back your Darth Vaders and inhibit the inflammation reaction in your body.
Problem is, the diet most of us subsist on today is more likely to strengthen our Darth Vaders than our Luke Skywalkers, and our good bacteria die out when there isn’t enough food for them. If we chow down on potato chips and French fries all the time, we’re fueling the Darth Vaders, who mow down everything in their path, Lukes included, and as a result our intestinal flora is knocked out of balance, our immune system is weakened, and inflammation arises.
Let’s look at things from a more positive viewpoint. The advantage of good bacteria is that when they exist in an environment in which they thrive, they’re able to defend us from inflammation and disease-causing bacteria. We just need to give them enough nourishing food (vegetable fibers, antioxidants, minerals, and good fats), and they’ll quickly grow strong and multiply.
Beneficial bacteria have many important tasks besides chasing out nasty bacteria. For example, they line the intestinal wall and ensure that toxins and other waste don’t leak out into the bloodstream and into the rest of the body. Imagine that your gastrointestinal tract is like a long, winding, amusement-park water slide through your body, and that Luke’s army extracts all the antioxidants, vitamins, amino acids, and minerals that you send down the chute to release nutrients into your body. Thanks to the slide’s enclosed system, substances that Luke’s army doesn’t need or want—the debris, toxins, and dead bacteria—can simply leave the body.
Where in the body is food absorbed?
Nutrients we ingest from food eventually leave the intestinal tract and make their way into the bloodstream to be moved to the body cells. However, the question is where are they absorbed—directly from the small intestine, or a few hours later from the large intestine (colon)?
Raw vegetables are exceptionally hard to digest, and as a result they travel all the way down to the colon. Once there, they dole out nutrients to our good Luke Skywalkers and defend us from inflammation. Unfortunately, most of the food we eat today is neither raw nor slow to digest. On the contrary, most of our daily food—white bread, pasta, and rice, for instance—is already taken up in the small intestine. Food that is processed, treated with pesticides, and lacking in fiber = a real cocktail of inflammation factors.
When we consume food that gets absorbed in the small intestine, our protective bacteria in the colon don’t get any of the fiber-, mineral-, and antioxidant-rich nutrients they need. You’ll recall that antioxidants are our body’s foremost protectors against free radicals and that they guard us from inflammation, illness, and premature aging. Without those antioxidants, free radicals are free to wreak havoc. In short order, this means a lowered immune system that’s plagued by lingering colds, and in the long run it could lead to worse. Food that is absorbed in the small intestine elevates blood sugar levels too fast, and this in turn overburdens our digestive organs—the liver and the pancreas—because they are put under stress when dealing with the excess sugar in the blood (which causes inflammation) as quickly as possible.
The enemies of gastrointestinal flora
From Figure 2 below, we can see clearly how, in the Western part of the world, we have decimated large sections of our intestinal flora. Westerners (the yellow line) have lost 40 percent of their intestinal flora compared to the Yanomami, an indigenous population of the Amazon (the green line), and 20 percent compared to countries where the population consumes a diet somewhere between ours and the Yanomami’s.

The Yanomami have lived without any contact with the modern world and have thus held on to their rich intestinal flora, which means that they hardly ever suffer from inflammatory conditions. In countries that have adopted a Western lifestyle, we can see high rates of chronic illness, which is caused by inflammation and bad intestinal flora. Processed food, along with little exercise and lots of stress, has depleted our intestinal flora and disturbed the balance of good and bad bacteria. Other studies show that today’s children and young people often have difficulty building protective intestinal flora because, among other things, they don’t eat a diet that encourages its growth. Projections indicate that rates of most chronic diseases will triple or even quadruple by the year 2050. In Sweden, research has shown that every other Swede will be affected by cancer at some point during his or her lifetime (currently, the ratio is one out of three).
Another major threat to gut health: antibiotics. Aside from knocking out the good bacteria in the intestinal flora, excessive use of antibiotics has led to emerging problems with multidrug-resistant bacteria. This is called antibiotic resistance, and it is one of the biggest dangers facing our health today. Antibiotic resistance means that bacteria have developed to a point where no antibiotic can fight it. As modern-age travelers crisscross the planet, antibiotic resistance is becoming a global concern. For instance, antibiotic-resistant bacteria that develops in India could quickly affect someone in America, and ominous forecasts show that more people will die from multidrug-resistant bacteria than from cancer within the next twenty years. Scientists warn us that if we don’t turn this situation around, multidrug-resistance will be the main cause of mortality by 2050.
So, use caution with antibiotics. If you’re in a situation in which you need to take a course of antibiotic drugs, boost your Lukes with supplements of good bacteria (i.e., probiotics or synbiotics) over the course of treatment, as well as for a few days after you finish your medication. Feel free to add an extra spoonful of fermented vegetables to each meal, and eat more raw vegetables than you typically would.


Shares