The Conversation is running a series of dispatches from clinicians and researchers operating on the front lines of the coronavirus pandemic. You can find all of the stories here.
As the omicron variant brings a new wave of uncertainty and fear, I can't help reflecting back to March 2020, when people in health care across the U.S. watched in horror as COVID-19 swamped New York City.
Hospitals were overflowing with sick and dying patients, while ventilators and personal protective equipment were in short supply. Patients sat for hours or days in ambulances and hallways, waiting for a hospital bed to open up. Some never made it to the intensive care unit bed they needed.
I'm an infectious disease specialist and bioethicist at the University of Colorado's Anschutz Medical Campus. I worked with a team nonstop from March into June 2020, helping my hospital and state get ready for the massive influx of COVID-19 cases we expected might inundate our health care system.
When health systems are moving toward crisis conditions, the first steps we take are to do all we can to conserve and reallocate scarce resources. Hoping to keep delivering quality care – despite shortages of space, staff and stuff – we do things like canceling elective surgeries, moving surgical staff to inpatient units to provide care and holding patients in the emergency department when the hospital is full. These are called "contingency" measures. Though they can be inconvenient for patients, we hope patients won't be harmed by them.
But when a crisis escalates to the point that we simply can't provide necessary services to everyone who needs them, we are forced to perform crisis triage. At that point, the care provided to some patients is admittedly less than high quality – sometimes much less.
The care provided under such extreme levels of resource shortages is called "crisis standards of care." Crisis standards can impact the use of any type of resource that is in extremely short supply, from staff (like nurses or respiratory therapists) to stuff (like ventilators or N95 masks) to space (like ICU beds).
And because the care we can provide during crisis standards is much lower than normal quality for some patients, the process is supposed to be fully transparent and formally allowed by the state.
What triage looks like in practice
In the spring of 2020, our plans assumed the worst – that we wouldn't have enough ventilators for all the people who would surely die without one. So we focused on how to make ethical determinations about who should get the last ventilator, as though any decision like that could be ethical.
But one key fact about triage is that it's not something you decide to do or not. If you don't do it, then you are deciding to behave as if things are normal, and when you run out of ventilators, the next person to come along doesn't get one. That's still a form of triage.
Now imagine that all the ventilators are taken and the next person who needs one is a young woman with a complication delivering her baby.
That's what we had to talk about in early 2020. My colleagues and I didn't sleep much.
To avoid that scenario, our hospital and many others proposed using a scoring system that counts up how many of a patient's organs are failing and how badly. That's because people with multiple organs failing aren't as likely to survive, which means they shouldn't be given the last ventilator if someone with better odds also needs it.
Fortunately, before we had to use this triage system that spring, we got a reprieve. Mask-wearing, social distancing and business closures went into effect, and they worked. We bent the curve. In April 2020, Colorado had some days with almost 1,000 COVID-19 cases per day. But by early June, our daily case rates were in the low 100s. COVID-19 cases would surge back in August as those measures were relaxed, of course. And Colorado's surge in December 2020 was especially severe, but we subdued these subsequent waves with the same basic public health measures.
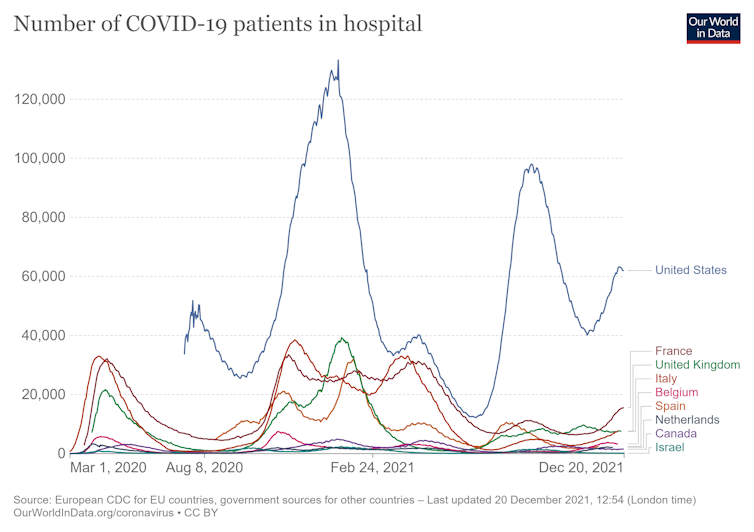
Number of COVID-19 patients hospitalized from Feb. 24, 2020 to Dec. 20, 2021. Our World in Data.org, CC BY
And then what at the time felt like a miracle happened: A safe and effective vaccine became available. First it was just for people at highest risk, but then it became available for all adults by later in the spring of 2021. We were just over one year into the pandemic, and people felt like the end was in sight. So masks went by the wayside.
Too soon, it turned out.
A haunting reminder of 2020
Now, in December 2021 here in Colorado, hospitals are filled to the brim again. Some have even been over 100% capacity recently, and a third of the hospitals expect ICU bed shortages during the last weeks of 2021. The best estimate is that by the end of the month we'll be overflowing and ICU beds will run out statewide.
But today, some members of the public have little patience for wearing masks or avoiding big crowds. People who've been vaccinated don't think it's fair they should be forced to cancel holiday plans, when over 80% of the people hospitalized for COVID-19 are the unvaccinated. And those who aren't vaccinated … well, many seem to believe they just aren't at risk, which couldn't be further from the truth.
So, hospitals around our state are yet again facing triage-like decisions on a daily basis.
In a few important ways, the situation has changed. Today, our hospitals have plenty of ventilators, but not enough staff to run them. Stress and burnout are taking their toll.
So, those of us in the health care system are hitting our breaking point again. And when hospitals are full, we are forced into making triage decisions.
Ethical dilemmas and painful conversations
Our health system in Colorado is now assuming that by the end of December, we could be 10% over capacity across all our hospitals, in both intensive care units and regular floors. In early 2020, we were looking for the patients who would die with or without a ventilator in order to preserve the ventilator; today, our planning team is looking for people who might survive outside of the ICU. And because those patients will need a bed on the main floors, we are also forced to find people on hospital floor beds who could be sent home early, even though that might not be as safe as we'd like.
For instance, take a patient who has diabetic ketoacidosis, or DKA – extremely high blood sugar with fluid and electrolyte disturbances. DKA is dangerous and typically requires admission to an ICU for a continuous infusion of insulin. But patients with DKA only rarely end up requiring mechanical ventilation. So, under crisis triage circumstances, we might move them to hospital floor beds to free up some ICU beds for very sick COVID-19 patients.
But where are we going to get regular hospital rooms for these patients with DKA, since those are full too? Here's what we might do: People with serious infections due to IV drug use are regularly kept in the hospital while they receive long courses of IV antibiotics. This is because if they were to use an IV catheter to inject drugs at home, it could be very dangerous, even deadly. But under triage conditions, we might let them go home if they promise not to use their IV line to inject drugs.
Obviously, that's not completely safe. It's clearly not the usual standard of care – but it is a crisis standard of care.
Worse than all of this is anticipating the conversations with patients and their families. These are what I dread the most, and in the last few weeks of 2021, we've had to start practicing them again. How should we break the news to patients that the care they are getting isn't what we'd like because we are overwhelmed? Here's what we might have to say:
"… there are just too many sick people coming to our hospital all at once, and we don't have enough of what is needed to take care of all the patients the way we would like to …
… at this point, it is reasonable to do a trial of treatment on the ventilator for 48 hours, to see how your dad's lungs respond, but then we'll need to reevaluate …
… I'm sorry, your dad is sicker than others in the hospital, and the treatments haven't been working in the way we had hoped."
Back when vaccines came on the horizon a year ago, we hoped we'd never need to have these conversations. It's hard to accept that they are needed again now.
Matthew Wynia, Director of the Center for Bioethics and Humanities, University of Colorado Anschutz Medical Campus
This article is republished from The Conversation under a Creative Commons license. Read the original article.



Shares