It came for us one by one, like a calculating antagonist in an Agatha Christie novel. I came home from a morning supermarket trip to find my spouse hunched at the dinner table, clutching a piece of plastic with two clear pink lines on it. "I have some not great news," he said.
That's how it started. But I had never had COVID, so I'd foolishly assumed I never would get it. Then I woke up in the middle of the night with a fever and a hacking cough. It hit my kids, home for winter break, next. First the younger one and then her big sister. One afternoon in the midst of it, I woke up sweat-soaked from a long nap to find one daughter sprawled in fitful sleep on the couch, her father similarly splayed facedown on the floor. In those early hours, our apartment didn't resemble a sick house so much as a crime scene. A few days later, I was so wracked with chest pains and shortness of breath that I had to get x-rays and lab work to rule out pneumonia or a blood clot. Now, weeks later, I'm still coughing. And after three years of living inside of a pandemic, after all the vaccines and boosters I've had and all the hand washing and mask-wearing I've done, I have learned firsthand this winter how much abrupt havoc COVID can still wreak, and why this year's version is unique.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter The Vulgar Scientist.
"The omicron subvariant XBB1.5 is by far the most contagious strain we've seen thus far," says Alice Benjamin, a clinical nurse specialist and the Chief Nursing Officer for Nurse.org. "It is quickly displacing the other omicron variant cousins BQ.1 and BQ.1.1, which dominated a wave of infections over the fall. Omicron variants and sub-variants have acquired both the ability to evade antibodies and an enhanced ability to infect human respiratory cells, making them more adept at spreading from person to person," she explains. Even people who managed to avoid getting sick until now.
"I had COVID for the first time in December, and flu as a bonus," my colleague Patricia told me recently, noting, "It kicked my butt for three-plus weeks, even with Paxlovid." And shortly after missing a get-together with a visiting friend because I had been too sick, she emailed me to say, "About COVID… I have it! Tested positive first day back from the trip. First time. I've managed to duck it for three years," she observed wryly, "but I guess it comes for all of us eventually." That doesn't make the fact that this far in, it's still coming for all of us any less hard to take.
"Unfortunately, we're still seeing lots and lots and lots of cases."
"It appears to me that the entire country has just moved on," says Dr. Shoshana Ungerleider, a San Francisco internal medicine physician and the founder of the end of life organization End Well. "Unfortunately, we're still seeing lots and lots and lots of cases."
On the day I tested positive, 756 people in the U.S. died of COVID, and there were 158,000 new cases reported. That number is likely only a small portion of the true count.
"We've stopped doing the necessary level of intake of information at the state level, certainly at the federal level to know just what's going on," says Dr. Ungerleider. My experience bears that out — my daughters hadn't needed medical attention, so 50% of our own household's COVID cases went uncounted.
For many, getting COVID isn't a matter of if but when — or when again. A December study in Morbidity and Mortality Weekly Report estimates that 42% of adults in America have already had the virus — a figure that's only going to increase over time. Given its prevalence, caution can feel like a Sisyphean endeavor. In the most miserable depths of my recent illness, I wondered whether the time I'd spent going for walks with friends instead of coming over for dinner, and the endless expense and effort of hand sanitizer spraying and counter wiping, had just been a futile attempt to outrun something that was always going to catch up with me anyway. I felt, frankly, pretty cheated.
In almost-hindsight, though, I know it could have been much worse. Last summer (before the emergence of the latest variant) the Mayo Clinic advised, "Fully vaccinated people with a breakthrough infection are less likely to have serious illness with COVID-19 than those who are unvaccinated. Even when vaccinated people develop symptoms, they tend to be less severe than those experienced by unvaccinated people." Maybe if I'd never been vaccinated and hadn't kept up with my boosters and flu shots I would have become exactly as horrendously sick as I truly was. I'm extremely relieved, however, that I didn't have to find out. I'm glad the rest of my family was sick for only a short span of time.
"It's really, really important to get updated boosters."
As long as this thing keeps spreading and evolving, continued common sense still remains the wisest option for protecting ourselves and our vulnerable loved ones from getting COVID or becoming seriously ill from it. First and foremost, "It's really, really important to get updated boosters," says Dr. Ungerleider. While 80% of Americans have been vaccinated against COVID, only 34% of us are fully boosted.
"Immunity wanes over time over the course of months, and these new sub-variants actually have a different genetic makeup than the previous variants," says Dr. Ungerleider. "Just because you had COVID, whether it was back in 2020, 2021, or 2022, it doesn't mean you can't get it again. I think people get relaxed, thinking, 'I got COVID before, so I am good.' It's just not that's not the case, unfortunately." She adds, "There's still a lot we don't understand about the long COVID picture. Who gets it? Why do they get it? Why does it affect certain people differently than others? How do we treat it? We don't know."
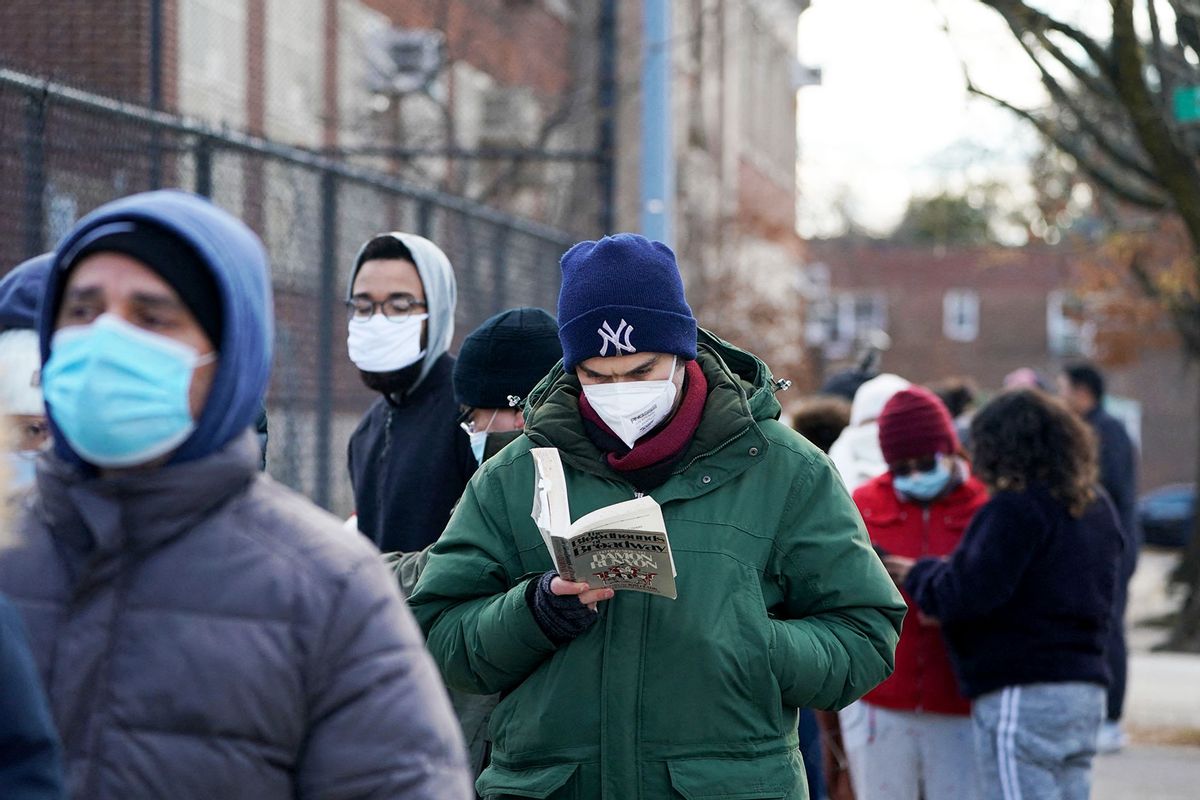
Beyond staying up to date with vaccinations, you probably know what else to do. "To have a safer season we need to stay diligent about washing our hands," says Alice Benjamin, "wearing a mask in crowded indoor spaces, practicing cough hygiene, testing for COVID, staying home if positive, and staying in good health overall."
And if you can, keep the clean air flowing. "To decrease the chances of a superspreader event in your home when entertaining a group, add a portable air filter to the space," says infectious disease epidemiologist and Infectious Economics founder and CEO Dr. Blythe Adamson. She says. "There are many reasonably priced portable HEPA filters available on Amazon with prices ranging from $50-150. The size or number needed depends on the square footage of your room."
While I am as fed up with COVID as anybody can be, I also gratefully recognize that vaccines and treatments like Paxlovid mean that we are nowhere near the level of chaos and risk of those dark early days of the pandemic three years ago. "Despite the enhanced transmission rate, XBB1.5 is not causing an alarming increase in the overall number of hospitalizations or deaths," says immunology and virology expert Kirsten Hokeness, Ph.D., Director of Bryant University's School of Health & Behavioral Sciences. "While the numbers infected are high, the impact still appears to be manageable. This is likely due to cross reactivity of immune systems that combine from natural infections of a variety of strains as well as the vaccines and updated boosters. A large proportion of the population has some degree of protection, which can help fight the infection faster, and limit severity despite the individual variant's immune evasiveness."
So I'll take an experience that was bad over one that could potentially have been catastrophic. I'll keep washing my hands and wearing a mask on the subway. And I'll assume my last case of COVID was really just my first case of COVID.
"As much as we're tired of talking about it, thinking about it, having to plan around it," says Alice Benjamin, "this virus is not done with us."


Shares