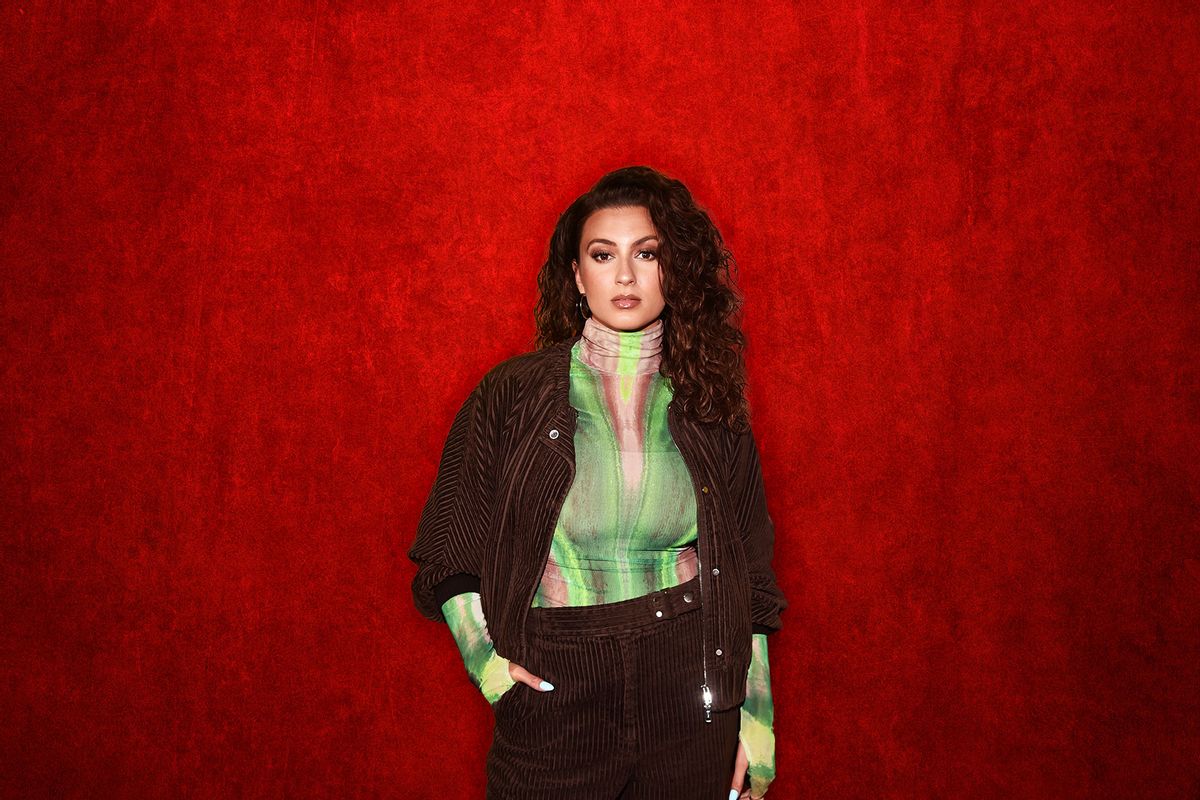
"It's been a scary few days," singer Tori Kelly said in a handwritten note shared on her Instagram page on July 27. Four days earlier, the Grammy winner had been out to dinner in Los Angeles when she felt her heart racing, and reportedly passed out. Her companions took her to Cedars-Sinai Medical Center, where, according to reports, the medical staff discovered blood clots in her legs and lungs.
Now, nearly a week later, her husband says she's "smiling and feeling stronger," but "not fully out of the woods yet." How could a young and and otherwise seemingly healthy wind up in such a crisis, so quickly?
While blood clots rarely get the attention that other health conditions like heart disease or diabetes do, they're a common — and sometimes fatal — issue. The CDC estimates that 900,000 Americans experience them per year, and 100,000 of them die. The National Clot Alliance puts the number of fatalities even higher, up to 300,000 individuals a year. (The number is tricky to pin down because blood clots can often accompany other health issues.)
That, as the National Clot Alliance notes, is considerably higher than the number of people who die of car accidents, AIDS or breast cancer. Yet few of us with direct experience of blood clots even know what they are, let alone how to recognize the warning signs.
"Being able to identify an active blood clot is important in medical treatment."
Anyone who's ever bled has some experience with clotting. As Tony Gilbert, a communications associate with the Masonic Medical Research Institute, a non-profit research center in Utica, explains, "A blood clot is simply a clump that occurs when blood hardens. When you cut yourself shaving, your body's nature response for blood clotting is actually preventing you from over-bleeding." He notes, "Blood clotting is not inherently bad or good, it all depends on the context."
For example, Gilbert says, "People with hemophilia are unable to clot blood properly, which means that even a minor cut can have serious consequences." And when a clot occurs inside the body, it can be life threatening.
We need your help to stay independent
When Tori Kelly had her health scare, the Los Angeles Times reported that her doctors "found blood clots around the 'Never Alone' singer's lungs and in her legs," and that "a medical team was working to determine if clots were present near the Grammy winner's heart." In a blood clots crisis, determining exactly where they are in the body, and then containing them, can become a race against time.
Another high risk factor is the increased estrogen brought on by hormonal birth control, pregnancy and childbirth.
"Being able to identify an active blood clot is important in medical treatment," Gilbert explains, "because an adult person has 60,000 miles of blood vessels in their body, which means that identifying the exact location of a blockage in that complicated system is crucial." He compares it to needing to find the scene of a traffic-blocking car accident on 60,000 miles of highway. "An imaging agent to identify blood clots is like a huge neon sign on the road pointing us to the exact location of the problem."
Clots in the veins, usually the arms or legs or pelvis, are known as deep vein thrombosis, or DVT. While they can happen to anyone at any time, lack of movement, even from sitting on long flights, can be a risk factor. More dangerous are clots that move to the lungs, causing pulmonary embolism, or to the heart, causing coronary thrombosis. Twenty years ago, NBC correspondent David Bloom died in Iraq of a pulmonary embolism. A blood clot that had started in his legs — perhaps due to his frequent traveling in cramped vehicles as a war correspondent — led to his sudden death at just 39.
Another high risk factor is the increased estrogen brought on by hormonal birth control, pregnancy and childbirth. Blood clots are a leading cause of maternal mortality in the United States, and the numbers have not gone down in the 20 years. Five years ago, Serena Williams revealed that she almost died of a pulmonary embolism after the C-section delivery of her daughter. Williams was, fortunately, proactive about her symptoms. "Because of my medical history with this problem, I live in fear of this situation," she wrote at the time. "When I fell short of breath, I didn't wait a second to alert the nurses… I am lucky to have survived."
Time is of the essence with blood clots — and it helps to have good guidance and good instincts. When I heard earlier this week about Tori Kelly's situation, I was thrust right back to the day my friend Kira calmly texted me that her arm was swollen and her doctor had recommended she go to the hospital. Because she'd been treated for breast cancer a few years earlier, she'd initially thought her symptoms might have been related to lymphedema.
Instead, by the time I met up with her in the emergency department, her doctors were scrambling to make sure that the clot in her subclavian vein under her collarbone wasn't moving toward her heart. "It didn't hurt," she recalls now. "It just felt a little bit strange and looked a little bit strange."
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter The Vulgar Scientist.
Without her history of breast cancer, Kira might have been tempted to put off medical attention until the situation had become far more dire. "The people in the ER told me, 'Your case is the most serious thing we're dealing with right now,'" she says. "I was like, 'I feel fine.' And then I was in the hospital for three days." She was fast tracked for surgery to remove the clot, and for three months afterward, she says she "couldn't really use my dominant arm."
The risk factors for blood clots can be mysterious and the symptoms difficult to identify, but there are some things to be on the lookout for the minimize the chances of getting them or being seriously affected by them. Blood clots can happen to anybody, at any time, but people with heart disease, obesity, smokers and those with a family history of blood clots are higher risk.
Likewise, while the exact causes aren't known, early research suggests people who've had COVID-19 are at "significantly" higher risk of venous thromboembolism. Earlier this year, when I had a case of COVID so severe I felt like a felt like a fish flopping on a hook, I had to go for X-rays twice to rule out pneumonia and pulmonary embolism. Like Kira, I already knew I had a higher chance of blood clots because I have a history of cancer — in my case one that metastasized into my lungs.
Early research suggests people who've had COVID-19 are at "significantly" higher risk of venous thromboembolism.
So how do you know if you're experiencing a blood clot, and when to seek medical attention? Like my friend Kira did, take any unusual redness, swelling or tenderness in your legs or arms seriously — it could be an early warning sign of DVT. Sudden shortness of breath, chest pain, rapid heart rate or sudden light headedness or fainting — like Tori Kelly's reported symptoms — can be signs of a pulmonary embolism. Trust your gut: you know your body and if something doesn't feel right in it, listen to it and get it checked out.
Blood clots can move quickly and the after effects can linger long after treatment. But prompt action can save your life, and full healing is, eventually, possible. The Journal of Circulation assures that "Most patients with DVT or PE recover completely within several weeks to months without significant complications or long-term adverse effects."
Four years after my friend Kira's close call, she's healthy and has no further incidents or complications. And just a few days after her hospitalization, Tori Kelly shared to her fans that "I'm feeling stronger now & hopeful." Then she added, "Unfortunately there are still some things to uncover."


Shares