Viewers may recall the first season of “The Magic School Bus,” in which Ms. Frizzle and her class shrink to microscopic size and dive into a sick student’s throat to track down the virus giving him a fever — a more educational take on the 1966 film "Fantastic Voyage," which is roughly the same premise. While the idea of sending squads of humans into another person is a common sci-fi trope, a similar concept is inching closer to becoming a reality with the development of ultra-tiny devices called nanoelectronics.
These machines, which are a mere one-billionth of a meter in size, are no larger than a mote of dust, truly living up to the name "nano." Originally proposed by physicist Richard Feynman in 1959, nanotechnology got a major boost when Austrian researchers developed the Scanning Tunneling Microscope, which zooms in to view surfaces at the atomic level, in 1981.
The global nanotechnology market is today valued at $57 billion, with the industry predicted to triple by 2028. The field has applications in everything from computer science to medicine to environmental science. We can thank this tech for helping shrink down room-sized computers to our cherished handheld devices. One environmental use involves introducing nanoparticles in the development of solar panels, which makes them more efficient. Yet one of the most popular and promising applications of nanoelectronics involves tiny devices that could one day enter the body to help cure disease.
Advances in nanotechnology on the horizon have the potential to completely revolutionize healthcare, said Dr. Sylvia Daunert, the director of the University of Miami’s Dr. John T. Macdonald Foundation Biomedical Nanotechnology Institute.
“We are going to be able to personalize medicine and repair tissues in ways that we were never able to do before,” Daunert told Salon in a video call. “We are going to help people live much longer with a better quality of life, and some diseases will become obsolete because we’ll be able to detect them early with this technology.”
"We are going to be able to personalize medicine and repair tissues in ways that we were never able to do before."
Some nanotechnology is already being used in medicine, like MRI contrast agents composed of magnetic nanoparticles. Other nanotechnology is being developed to deliver drugs in the body, which has the potential to reduce toxic effects and direct drugs to specific tissues or cells.
Some of Danuert's research involves designing nanoparticle systems that can help drugs get past the gut and into the bloodstream more efficiently and using nanoparticle sensors to detect bacteria causing inflammation in people with Chrohn's disease. Moderna and Pfizer used nanotechnology in the development of their mRNA vaccines, in which nanoparticles sheltered mRNA so it could be delivered to the body without triggering its immune response.
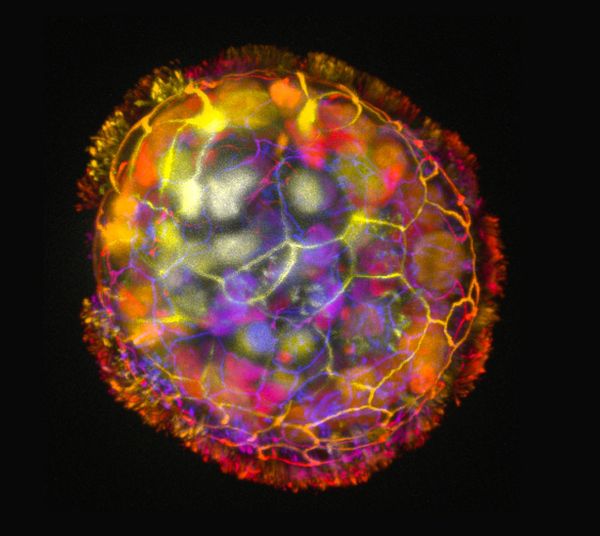 An Anthrobot is shown, depth colored, with a corona of cilia that provides locomotion for the bot. (Gizem Gumuskaya, Tufts University)
An Anthrobot is shown, depth colored, with a corona of cilia that provides locomotion for the bot. (Gizem Gumuskaya, Tufts University)
Getting a foreign object past the immune system, no matter how small, is one challenge to any medical nanoelectronic, said Brian Timko, an assistant professor of biomedical engineering who studies nanoelectronics at Tufts University.
“You also have to eliminate them somehow because you don’t want them getting stuck in the kidneys or accumulating in organs and lymph nodes, which can happen [with] some larger gold particles over two nanometers or so,” Timko told Salon in a phone interview.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter Lab Notes.
Although in its early stages, research published last month in Advanced Science proposed one way to get around the immune response challenge. A group from Tufts University developed tiny robots derived from human lungs that they call "anthrobots." These bots, no wider than a human hair, are designed to multiply and move about. The idea is that the body recognizes them instead of sending its immune system attackers to destroy them. In the study, researchers showed these bots not only successfully multiplied but traversed across a Petri dish to help reconstruct a damaged region of tissue on the other side.
“Anthrobots are derived from adult human tissue, and in the future could be personalized for each patient, enabling safe in-vivo deployment of these robots in the human body without triggering an immune response,” the authors wrote.
Questions remain about how these anthrobots could be targeted to specific tissues, and it’s a long way to go before something like this is tested in humans, Daunert said.
Still, as the authors wrote, this technology could one day be used for “clearing plaque buildup in the arteries of atherosclerosis patients, bulldozing the excess mucus from the airways of cystic fibrosis patients, and locally delivering drugs of interest in target tissues.”
Another challenge in developing these ultra-tiny devices is that any nanoelectronic designed to monitor the body also needs to be able to communicate with an external source. Then, there’s the challenge of organizing and detecting changes to the body with massive amounts of data, which artificial intelligence has the potential to help with.
“Beyond healthcare, this fusion of nanotechnology and cells can lead to unique living hybrid robots, opening up myriads of interesting applications.”
“There are many, many billions of neurons in the brain, and each neuron can have 1,000 or so synapses with other neurons, so there’s a lot of complexity there,” Timko said. "If you can get a whole bunch of devices in the brain, that’s good, but the signals are so complicated, how do you make sense of it?”
Although also in the early stages of research, a team from MIT is developing nanoelectronics they hope can one day enter the brain and treat conditions like Alzheimer’s by monitoring some of these brain patterns. Their device, which they call Cell Rover, serves as a sort of antenna that can help external devices monitor cells. In frog cells, the Cell Rover has been shown to successfully install itself in a living cell and connect to magnetic fields produced outside of the body.
The difference between Cell Rover and things like Elon Musk's Neuralink is that the latter is designed to control an external computer and still requires implantation — meaning the skull is opened to bacteria and potential infection when the device is injected.
It's not clear how the Cell Rover would be implanted in the body, but ideally, devices like these could travel up to the brain through the circulatory system and be less invasive. Once there, they could detect small changes in the body that go unnoticed in conditions like Alzheimer's, usually until too much degradation has occurred for anything to be done. One day, these machines could be programmed to not only detect threats in the body like tumors but even destroy them.
“This technology has the potential to not only provide fundamentally new insights into biology but also create novel pathways for health monitoring and therapeutics,” MIT researchers wrote in their study on Cell Rover. “Beyond healthcare, this fusion of nanotechnology and cells can lead to unique living hybrid robots, opening up myriads of interesting applications.”
If that becomes a reality, it’s still a distant one, Timko said. Some fundamental questions remain before many of these devices even reach the U.S. Food and Drug Administration and begin being tested in humans, like whether these electronics should be even considered devices or drugs, he added.
We need your help to stay independent
“Proving something is safe in humans close to 100% of the time is a big hurdle,” Timko said. “I think the field is headed in the right direction, but there is still a lot of work to do for clinical translation.”
At the same time, the recent explosion of artificial intelligence shows how fast technology can advance. And it seems a matter of when, not if, these devices will successfully be outfitted to target and treat disease in the body.
"If you can program these things to specifically target and attack a tumor or enter the brain and somehow mitigate the effects of Alzheimer’s, these are problems we just don’t know how to address right now,” Timko said. “Designing something biological that can do what you tell it to do — that’s huge.”


Shares