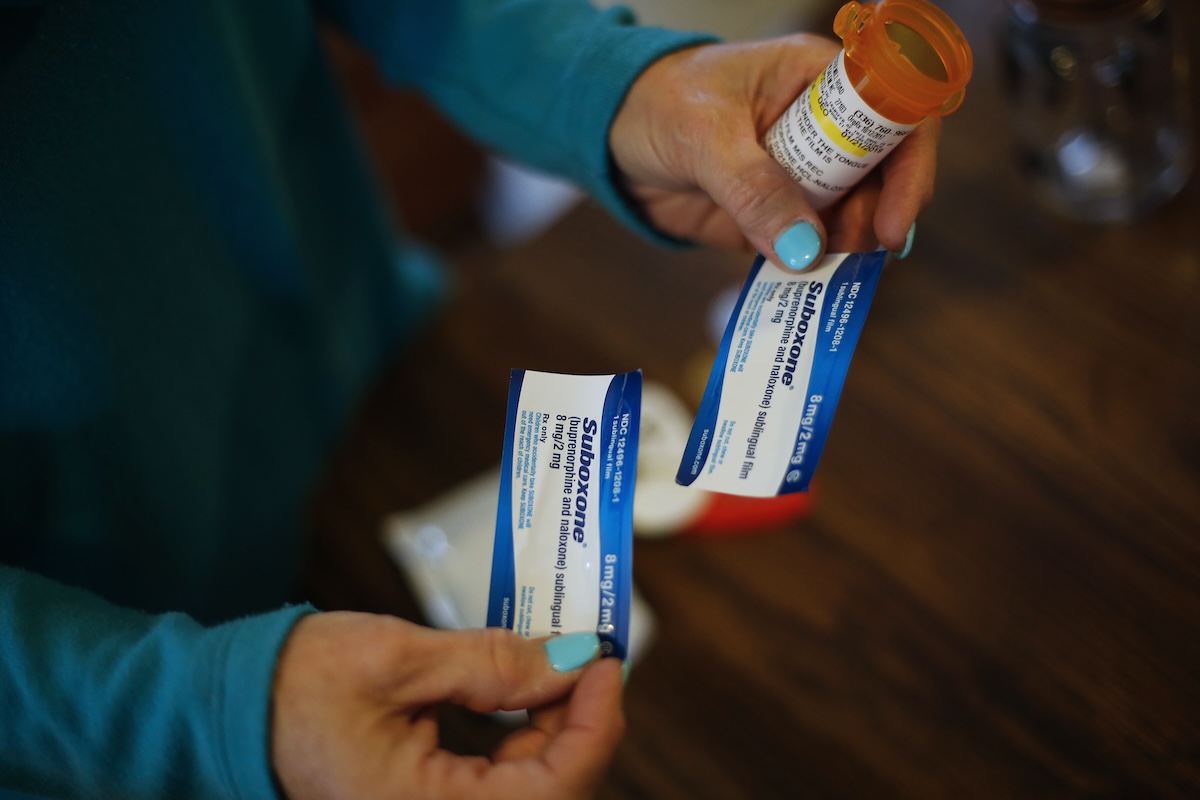
There’s a treatment for opioid use disorder (OUD) that literally saves lives. It has been proven to reduce the risk of overdose death by as much as 60% and reduce the risk of any cause of death by half. It is also one of the oldest and most rigorously studied treatments for opioid use disorder: medication treatment with methadone or buprenorphine (also known as opioid agonist treatment, or OAT).
Since the start of the overdose crisis, serious efforts have been made to expand the availability of OAT. Federal agencies have been proactively removing barriers to OAT and allocating resources to its expansion. OAT is also a core strategy that can be funded with the billions of dollars obtained by local communities through the global opioid settlement.
Despite all this, tens of thousands of people are still dying annually. Estimates suggest that the number of opioid overdose deaths declined in 2023, but just barely, with more than 80,000 US lives lost to opioids in a single year.
This past year, my colleagues and I set out to explore this contradiction: why, when we have treatments that are proven to prevent overdose death, are so many people still dying? To do so, we homed in on residential treatment centers across the state of North Carolina, where many North Carolinians living with OUD expect to receive guidance, support and – naturally – lifesaving medical treatment.
What we found, published recently in the Journal of Substance Use and Addiction Treatment, was staggering. After a four-month-long audit of private organizations across North Carolina advertising themselves as residential treatment centers, we found that only seven of those centers provided on-site access to OAT. Another nine allowed the use of OAT obtained through other providers. The remaining 49 centers – 74% percent of the organizations we identified – barred clients from receiving OAT while participating in their program. Moreover, more than half of the centers that were state-licensed providers of substance use services prohibited the use of these medications in their programs.
For too long, research-backed solutions to overdose deaths have been eschewed in favor of untested, ideological, punitive and moralistic measures.
The reason? When we called them to ask, most centers banning OAT told us these medications are “more addictive than illicit drugs,” that OAT is “bad for you,” and that OAT “will kill you.” These statements are factually incorrect. A few centers also gave prejudiced answers, describing OAT as “legal heroin,” “not true recovery,” or “just trading one addiction for another.” That’s a hard statement to swallow in the face of 80,000 deaths a year and decades of science demonstrating that OAT could cut those deaths in half.
According to the current, best practice treatment guidelines set by the American Society of Addiction Medicine (ASAM), residential care for substance use disorders must include “access to medications for [opioid use disorder] – made available on-site or in the immediate community.” Based on our recent findings, it’s clear that North Carolinians seeking treatment for opioid use disorder cannot expect to receive ASAM’s lifesaving, gold-standard of care from the majority of “residential treatment centers” across the state.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter Lab Notes.
Sadly, this broken treatment system is not isolated to North Carolina. A nationwide study recently found that only 1 in 4 of the nearly 10 million US residents living with opioid use disorder ever receive OAT. Right now, we’re losing more than 100,000 people to drug overdose every year, yet our treatment system is still broken, insufficient and years behind the curve.
What can be done to make lifesaving treatment available for everyone who needs it in North Carolina and elsewhere?
The first step policymakers can take is to tighten regulations on licensed residential treatment centers. Currently, North Carolina does not require licensed service providers to facilitate access to OAT. Updating the state’s licensing and Medicaid regulations to mandate facilitated access to OAT could substantially reduce overdose rates across the state. Moreover, state and local officials can rigorously enforce existing state laws that prohibit service providers who do not offer evidence-based treatments from giving the false impression that they do.
Second, North Carolina policymakers should take advantage of the approximately $1.5 billion in opioid settlement funds that will be distributed across the state in the coming years — funds that provide the state with a unique opportunity to expand access to lifesaving, evidence-based medication like OAT.
We need your help to stay independent
However, as of September 2024, fewer than one-third of local governments in North Carolina have released plans to expand access to evidence-based treatment. Instead, state and local leaders have allocated tens of millions of dollars to residential treatment centers that adopt strict anti-OAT or abstinence-only stances — a form of “treatment” recently shown to be worse for participants than no treatment at all. State and local leaders must take action to reverse this trend and ensure that these once-in-a-lifetime settlement funds are used to help — not hurt — North Carolinians.
For too long, research-backed solutions to overdose deaths have been eschewed in favor of untested, ideological, punitive and moralistic measures, leaving millions of Americans without the lifesaving treatment they need. Our research in North Carolina starkly reveals the dire situation for people with opioid use disorder. At the same time, these findings shine a light on how simple it can be – through steps like improving regulation, funding medication access, and enforcing existing laws – to reap the full, lifesaving impact of the most promising overdose prevention strategy available to us.
We can end overdose deaths — not just reduce them. Achieving this goal is within our reach, but only if we use the tools that actually work.
Read more
about drug policy