Pharmacies in the nation of Georgia have something ours don’t: vials of viruses in neat rows. People swallow or gargle the brews to combat routine bacterial infections. The viruses are bacteria-eaters that take on the human body’s enemies, sometimes with near-miraculous results. (Almost as amazing, kids even like the taste.)
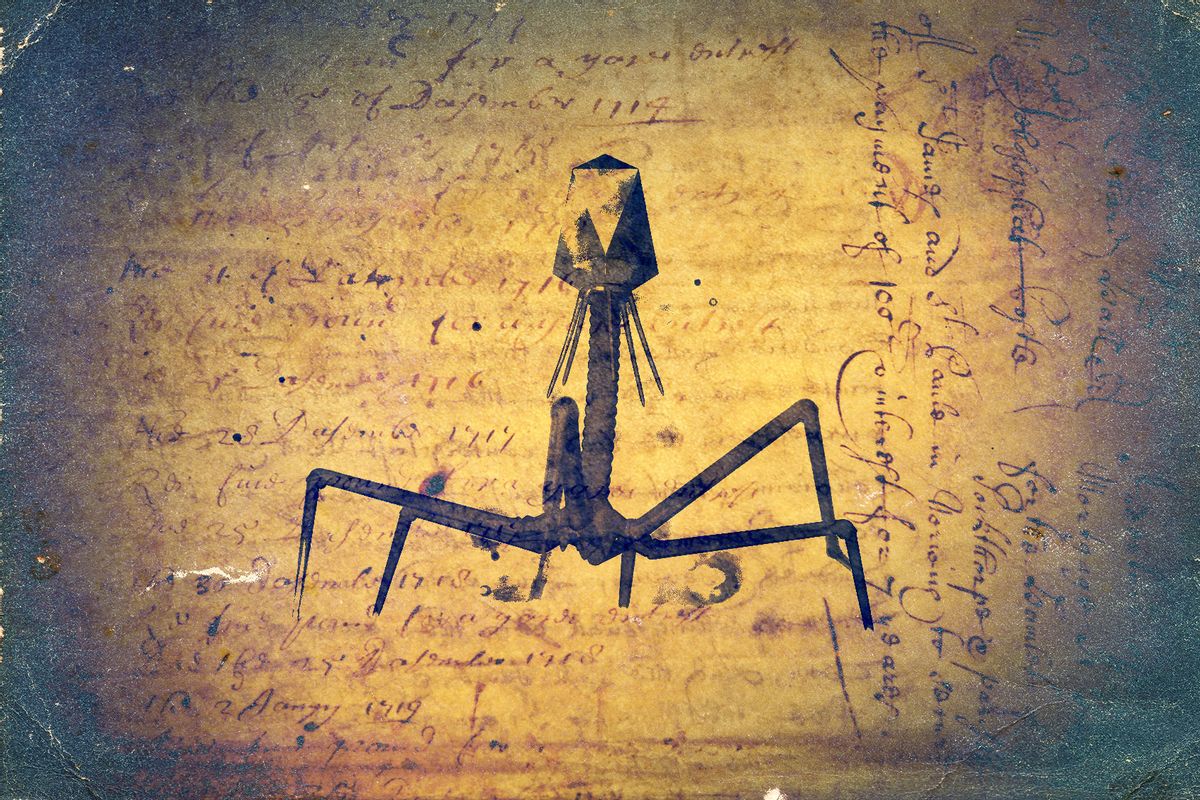
These medicines, called bacteriophages, were developed over much of the 20th century, primarily in Georgia and other parts of Europe and the former Soviet Union, by dedicated scientists who battled not just microbes but also doubtful colleagues and corrupt politics. Meanwhile, much of Western medicine went all-in on antibiotics in the 1940s.
But microbes with resistance to those antibiotics emerged by the 1950s. Today, resistant microbes appear, on average, within two or three years of a new drug’s release. More than 1 million people succumb to drug-resistant infections every year, and the death toll could reach nearly 2 million per year by 2050.
While new antibiotics continue to trickle out, medicine needs a radical solution, argues Lina Zeldovich in “The Living Medicine: How a Lifesaving Cure Was Nearly Lost—and Why It Will Rescue Us When Antibiotics Fail.” And that solution, she writes, has been sitting on the shelves of a bacteriophage institute in Tbilisi, Georgia, for decades. Unlike commercial antibiotics, phages evolve alongside their bacterial hosts, dodging and parrying the bacterial response so that for every pathogen, there’s likely a bacteriophage, somewhere, that eats it.
Zeldovich, a journalist who was born in the former Soviet Union, traces the history of phages from the early 20th-century recognition of their potential in Georgia and France to a nascent resurgence of interest in the U.S. today. Zeldovich details the personal stories of the men who first recognized phages’ potential before moving into their modern rediscovery and ongoing development in the U.S.
In places, the book is as much a history of 20th-century Soviet politics in Georgia as it is a science book. Much of the narrative stars the fathers of bacteriophage research, Georgian Giorgi Eliava and French Canadian Félix d’Hérelle.
Zeldovich describes d’Hérelle as self-taught and adventurous, if a bit abrasive. He was a lowly lab assistant at the Pasteur Institute in Paris when he first collected the data that would lead to the discovery of bacteriophages. It was the meticulous d’Hérelle who, along with his wife, came up with the term “bacteriophage.” He also penned the original text on developing bacteriophages for medical use.
Bacteriophages were developed over much of the 20th century by dedicated scientists who battled not just microbes but also doubtful colleagues and corrupt politics.
Eliava, in contrast, was a mischievous charmer who pranked his friends, once dressing as a woman to flirt with d’Hérelle at a dinner party, and kept sketchy notes in the lab. As Zeldovich describes it, his affair-turned-marriage with the opera singer Amelia Wohl-Lewicka makes up a chunk of his story.
Both men separately stumbled onto the bizarre bacteriophage phenomenon in the 1910s, when the bacteria they were growing mysteriously vanished. Other scientists disparaged d’Hérelle’s theory of the invisible killers, but Eliava, visiting the Pasteur Institute later that decade, recognized the finding and conducted further experiments that proved d’Hérelle was right. When the two met for the first time in the halls of the Institute, they immediately embraced, writes Zeldovich.
In Tbilisi, Eliava founded the laboratory that would eventually bear his name, the modern-day George Eliava Institute of Bacteriophages, Microbiology, and Virology. It was here that much of the work to turn his and d’Hérelle’s observations into workable medicines took place.
But Eliava played politics poorly. He angered the officials whom he circumvented to fund his work. His behavior backfired in 1937 when he and his wife were arrested amid Soviet purges. Tortured and accused of bizarre espionage plots, he was ultimately executed by firing squad. “Stalin’s purges were worse than any plague or infectious disease,” Zeldovich writes.
D’Hérelle, who had been poised to live and work in Georgia, then disappears from her narrative too; he died, largely forgotten, of cancer, in Paris in 1949. Others carried the torch of phage medicines onward. By the 1980s, hundreds of staffers at Eliava’s institute were mass-producing phage cocktails for medicine and agriculture.
If bacteriophages are so spectacular, why weren’t they adopted in the U.S. and many other Western nations?
In fact, phages did get a shot in the U.S. soon after their discovery. But they performed poorly. Phages are exquisitely specific for their bacterial targets, and some treatments were prescribed for the wrong infections. “Because making potent phages took considerable time and work, the quality often suffered,” Zeldovich writes.
By World War II, even as scientists were manufacturing gallons of phages to combat cholera, dysentery, and gangrene in Stalingrad and Leningrad, much the West had given up on phages. And the Iron Curtain, of course, divided biology and medicine as starkly as it did politics and cultures.
Plus, the West had antibiotics — which spread willy-nilly not just in medications, but in toothpaste, lipstick and, perhaps most dangerously, into farm animals to promote growth. The result: drug-resistant superbugs emerged as early as the 1950s. In North and South America, about 40 percent of deaths caused by bacterial infections in 2019 were associated with drug-resistant microbes, according to a 2023 study.
By World War II, much the West had given up on phages. And the Iron Curtain, of course, divided biology and medicine as starkly as it did politics and cultures.
That’s why phage therapy is starting to pique the interest of Western medicine again. Eastern scientists such as Alexander Sulakvelidze, one of Zeldovich’s main modern characters, who left Georgia after the fall of the Soviet Union, brought the message of phage’s potential.
But the very thing that make phages so promising — their ability to evolve in step with pathogens — has been their undoing at the Food and Drug Administration, at least until recently. Regulators expect medicines to be static entities they can test once and trust forever. “Living medicines don’t fit neatly into the FDA’s approval pathway,” Zeldovich explains. “That made it very difficult for phages to earn FDA approval.”
She attributes the new rise of interest in the U.S. in part to one very sick man: psychologist Thomas Patterson of San Diego. Patterson should have died from a nasty superbug picked up in Egypt in 2015 — except Patterson is married to bullheaded epidemiologist Steffanie Strathdee. She learned of phages and orchestrated Patterson’s treatment, as Zeldovich summarizes and Strathdee and Patterson chronicle in their own excellent book, “The Perfect Predator: A Scientist’s Race to Save Her Husband from a Deadly Superbug.”
Today, phages are getting a second shot in the U.S., and in other nations. For example, Sulakvelidze’s company Intralytix is running clinical trials targeting multiple kinds of infections, and Strathdee co-founded a center to support phage studies. “We spent twenty years educating the FDA about phages,” Sulakvelidze told Zeldovich. “And it finally paid off.”
The FDA, though now interested in phages, will have to figure out how to regulate them to keep up with evolving microbes.
Zeldovich spends less time on the hurdles these medicines still face. While phages can work handily when swallowed to treat stomach ailments, they’re more difficult to use for bloodstream or whole-body infections. The preparations, as Zeldovich notes, often contain remains of vanquished bacteria that, when injected, inflame the immune system and put the patient at risk. If phage treatment continues long term, patients can make antibodies against them. Phages are rapidly filtered out of the blood by the liver and spleen, but they can also reproduce, making it hard to determine the right dose.
Extremely sick patients like Patterson require bespoke phage cocktails that perfectly match their microbes, and may even need new phages as the bacteria evolve. It’s the ultimate in personalized medicine. Zeldovich describes but a handful of patients who have benefitted from such treatments thus far. And the FDA, though now interested in phages, will have to figure out how to regulate them to keep up with evolving microbes.
Zeldovich has spun a thrilling tale, but one hopes it’s just the beginning and middle of the story, with the climax of phage-fueled medicine yet to come. Indeed, as Zeldovich writes, “These phages might be our best weapons against the next bacterial pandemics.”
This article was originally published on Undark. Read the original article.




Shares