Zoe struggled with various mental health conditions in her childhood but was too young to be able to communicate what she was feeling. Struggling so much throughout her adolescence, she began to feel like there was something wrong with her. Over time, she internalized these negative feelings about herself and was diagnosed with anorexia when she was 14.
To treat her condition, Zoe’s parents decided to try something called family-based treatment, which is the standard of care for adolescents with anorexia nervosa or avoidant/restrictive food intake disorder (ARFID.) It essentially involves parents taking complete control of feeding their kids.
This is often the best-available treatment for adolescents in addition to having a multidisciplinary team of nutritionists, psychiatrists and pediatricians — but has been shown to only help 50% of people reach remission. It didn’t work for Zoe, who is only using their first name to protect their privacy. She says the experience damaged her relationship with her family and led to a distrust in the health care system she carries with her to this day.
“Honestly, it was just a nightmare that really did not work for me or my family,” Zoe says.
At least 9% of people in the U.S. are predicted to experience an eating disorder at some point in their lives, including anorexia nervosa, bulimia nervosa, binge eating disorder, or ARFID. That prevalence is increasing and particularly spiked during the COVID-19 pandemic, when emergency room visits associated with these conditions increased seven-fold.
Racial discrimination, bullying, sexism and other forms of discrimination have also been shown to increase the risk for eating disorders.
The pandemic-related isolation that sent many adolescents home with their parents during this period was challenging developmentally, said Dr. Tracy Richmond, a pediatrician and director of the Eating Disorders Program at Boston Children’s Hospital. The isolation, uncertainty, and disruption to children’s daily lives likely exacerbated these conditions, like it did many other mental health conditions.
“We've had patients who have remained ill for years,” Richmond told Salon in a phone interview, saying the pandemic “was just an unbelievable psychic wound.”
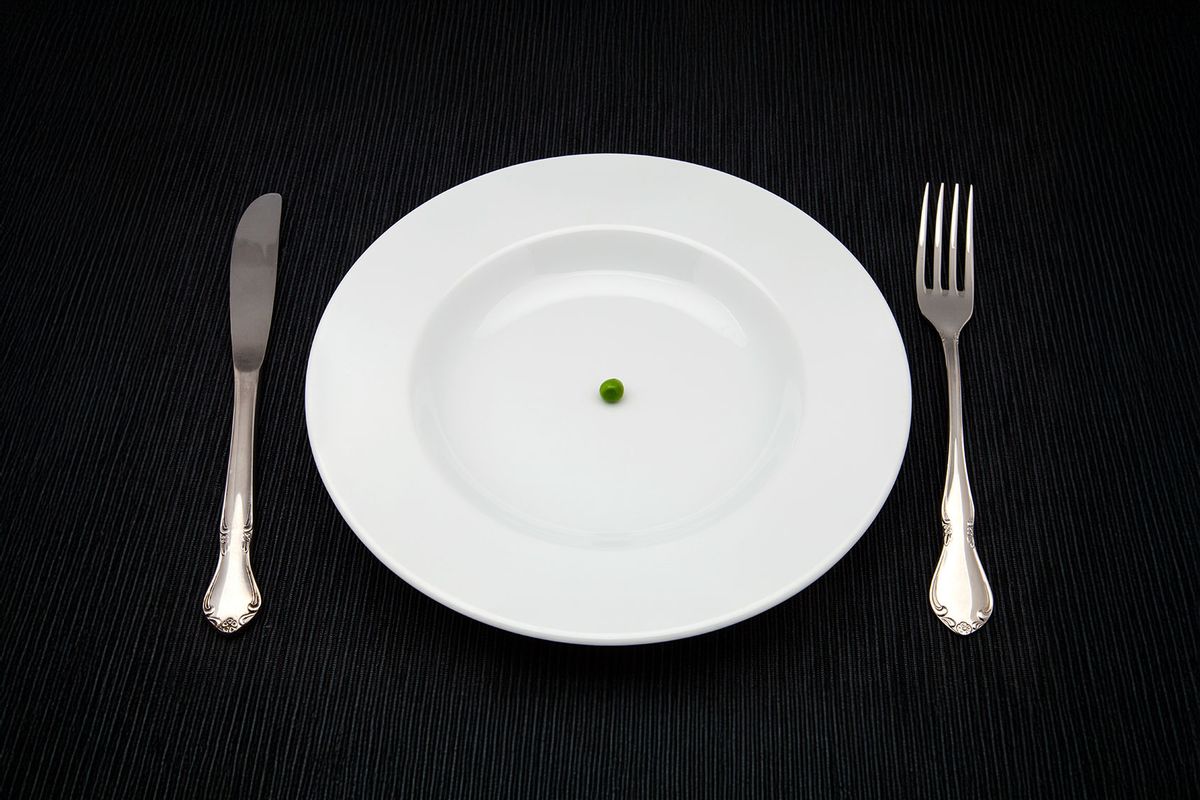
Each eating disorder is unique and comes with its own treatment recommendations. These are often complex conditions where people might have multiple co-occurring mental health conditions, a history of trauma, or face treatment barriers. These disorders are mental health conditions that also inherently affect the physical body and can lead to consequences on organ systems along with the brain, which further complicates care. Treatment is also often complicated because people with eating disorders are required to face the food that might trigger them every day in order to get the nutrients they need to survive, and one of the diagnostic criteria for anorexia, for example, is failing to recognize the seriousness of illness.
Want more health and science stories in your inbox? Subscribe to Salon's weekly newsletter Lab Notes.
However, the stakes are high to get people care. Eating disorders are the second most deadly mental health condition behind substance use disorder — but only half of people with these conditions will receive treatment in their lifetimes. Part of the reason is that specialized treatment centers are limited in number and capacity, especially in rural areas. Stigma is also still deeply seeded in these conditions, which have traditionally been associated with affecting affluent white girls.
Yet the reality is that eating disorders affect people in all sociodemographic groups, including people with higher weights, men and people of color. In fact, bulimia and binge eating disorder have been shown to disproportionately affect Latina girls, whereas eating disorders have been shown to disproportionately affect people who are experiencing food insecurity and LGBTQ youth, especially the trans community.
Racial discrimination, bullying, sexism and other forms of discrimination have also been shown to increase the risk for eating disorders, said Dr. Ariel Beccia, an epidemiologist at Boston Children's Hospital who works with the Strategic Training Initiative for the Prevention of Eating Disorders.
“There are really, really large barriers to care experienced by youth of color more broadly, and that, in turn, can exacerbate inequities by prolonging the course of an eating disorder and exacerbating symptoms,” Beccia told Salon in a phone interview.
For those who do access treatment, the options are relatively limited. Depending on the condition, it may include antidepressants or off-label pharmacological options, as well as psychological interventions like cognitive behavioral therapy, family therapy, or specialized protocols for certain eating disorders. If the illness is more severe, patients can also enter outpatient, inpatient or residential facilities offering these services to get care, although these can cost thousands of dollars per day and are not always covered by insurance.
“Our insurance systems separate medical care from behavioral healthcare, so individuals usually land in one or the other,” said Dr. Evelyn Attia, a professor of psychiatry at Columbia University and Weill Cornell Medical who has spent 30 years treating patients with eating disorders. “The idea that you need expertise from both isn’t fully understood by the systems as they are currently built.”
Throughout the rest of her teenage years, Zoe’s eating disorder progressed and she was hospitalized several times. Since she was diagnosed, Zoe has tried seven different inpatient and outpatient methods with different approaches to try and treat her anorexia. Some helped her get back to school and her life for a time, and she could tell that the people working there were really trying to help. But nothing helped her reach any kind of remission.
“A theme that I’ve experienced a lot in various care for my eating disorder is that it always feels like a me-versus-them kind of situation where I feel like we should all be on the same side trying to help me overcome my eating disorder,” Zoe said. “Part of that is understandable because eating disorders, especially anorexia, tend to be disorders that the patient wants to defend and feels very ambivalent about getting better … But they are also disorders that carry so much shame, and I think instilling a greater sense of shame and fear in the patient is really not the right way to go about it.”
"Instilling a greater sense of shame and fear in the patient is really not the right way to go about it."
Treatment got even more difficult to access as an adult, and she spent months on waitlists trying to get to publicly funded care centers in Canada. The private centers she came across were very expensive and often had stricter requirements that patients had to meet, like having a certain body mass index (BMI), she said.
“You have to be above a certain BMI, or you have to be kinetically stable, or you have to be not engaging in certain behaviors, or you have to be willing to eat certain foods to be in the program,” Zoe said. “I was kind of caught in this place of being too sick for some programs and not sick enough for others.”
Part of the reason there are so few treatment options is that research efforts to find more effective treatments and better understand the needs of people with eating disorders are chronically underfunded. One study showed the number of federal dollars going toward eating disorder research each year totaled $0.73 per patient. For comparison, $58.65 went toward each patient with autism and $86.97 went toward each patient with schizophrenia.
“This is a very understudied population with very little guidance [on] treatment,” Richmond said. “Even the guidelines a lot of times are based on consensus rather than evidence … And there aren't these large-scale studies that really can help us know exactly which treatment to do for which groups.”
Some of the most critical questions in national surveys used to assess youth’s risk for eating disorders have also been removed in the past decade. In 2015, the Youth Risk Behavior Survey (YRBS) run by the Centers for Disease Control and Prevention (CDC) removed questions about fasting, diet pill use, and purging.
“Lacking that basic data has a ton of downstream consequences,” Beccia said. “You need that data when you’re talking to policymakers about why this matters and why we need more money for treatment, or when you are submitting grant applications to the National Institutes of Health or other big funders to say: This is a public health issue and we need money to do research.”
We need your help to stay independent
Eating disorders are also often left out of medical training, especially for providers specializing in things like family or internal medicine. In one 2014 study, about one-quarter of more than 500 accredited graduate medical training programs offered elective rotations for eating disorders, and just 8% offered a formally scheduled rotation. However, this is a huge missed opportunity to reach people with eating disorders before their condition progresses to the level of needing inpatient care, Attia said.
“These are also illnesses that often need a multidisciplinary team, so it's a range of folks who need training, whether it's for that early intervention piece or later on, teams of mental health providers, medical health providers, dieticians, and others who really work together with individuals with these particularly threatening conditions,” Attia said.
Efforts are underway to connect people with eating disorders to better care. Attia designed a curriculum for medical professionals to familiarize themselves with eating disorders so that they can better recognize and treat people with these conditions. For the 2025 YRBS, the CDC added a binge eating item following advocacy efforts by researchers. And some are advocating for further research exploring a harm reduction approach to eating disorders.
"Lacking that basic data has a ton of downstream consequences."
After Zoe’s most recent hospitalization, she felt burnt out by treatment and discharged against medical advice. She went about a year without receiving any form of treatment before she started seeing a therapist who used this harm reduction approach in sessions. Although Zoe was going to therapy to work through some other things and didn’t intend on talking about her eating disorder, it naturally came up in sessions.
“In that environment of trust and safety … slowly but surely I actually started wanting to talk about my eating disorder and I actually started wanting to make changes,” Zoe said.
Zoe still sees her condition as severe but has remained medically stable since she started seeing her therapist. She has been able to go back to university and get a job as a barista. More importantly, she has a desire to live that has been absent for the last five years, she said.
“I guess it’s going to take some time to figure out what exactly living is going to look like for me because I honestly never imagined that I would make it to this point, much less imagining a decade or two or three down the line,” Zoe said.
It may not be an easy journey, and Zoe doesn't know if she will ever be fully recovered, or what that means for her, she said. But she has taken steps toward recovery this past year she hasn't taken since she received her diagnosis — steps she didn't in the past think she was even capable of.
“Recovery is a hard thing to define,” she added. “I think at the end of the day, we’re all just trying to survive and figure out our lives and exist comfortably in this world. That’s going to look really different for everyone.”


Shares